The inter-relationships between health and social determinants such as education, employment status, overcrowding and income are well established in the national and international literature (Marmot, 2015).
In turn, health influences educational participation and attainment. For example, the Longitudinal Study of Indigenous Children has found 83 per cent of Indigenous children with better health attended school at least 80 per cent of the time compared with 65 per cent of the time for children with poorer health. Similarly, poor health adversely affects employment (Holzinger and Biddle, 2015).
target
Close the gap in life expectancy between Indigenous and non-Indigenous Australians within a generation (by 2031).- While Indigenous mortality rates have declined by 16 per cent since 1998, we are not on track to close the gap in life expectancy by 2031 and it is important to accelerate progress.
- Since 1998, there have been significant improvements in the Indigenous mortality rate from chronic diseases, particularly from circulatory disease. However, Indigenous cancer mortality rates are rising and the gap is widening.
- There have been improvements in healthcare access and reductions in smoking which should result in long-term improvements in the health of Aboriginal and Torres Strait Islander peoples.
- Working collaboratively across governments, the health sector and with Aboriginal and Torres Strait Islander communities on local and regional responses is central to the Government’s approach to improve life expectancy.
- Recognising Aboriginal and Torres Strait Islander people experience higher rates of mental health issues than other Australians, the Government is improving access to culturally sensitive, integrated mental health services.
What progress is being made?
The health of Aboriginal and Torres Strait Islander people is slowly improving but the current rate of progress will have to gather pace if the life expectancy target is to be met by 2031. Meeting this target remains challenging because, among other things, non-Indigenous life expectancy is expected to rise over the coming years. This means, for example, Indigenous life expectancy will probably have to increase by almost 21 years for males and 16 years for females from 2006 to 2031 to meet the target. Average annual Indigenous life expectancy gains of between 0.6 and 0.8 years are needed.
The most recent life expectancy figures were published in late 2013 and have featured in the last two Closing the Gap reports. In 2010-12, Indigenous life expectancy was estimated to be 69.1 years for males and 73.7 years for females, a gap of 10.6 years for males and 9.5 years for females (see Figure 10). Between 2005-07 and 2010-12, there has been a small reduction in the gap of 0.8 years for males and 0.1 years for females. Health outcomes for Indigenous Australians are often worse in remote areas than in urban and regional areas 28.
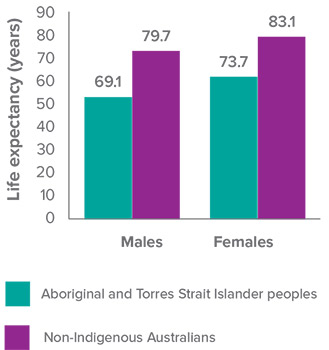 Source: ABS (ABS, 2013)
Source: ABS (ABS, 2013)
While official Indigenous life expectancy estimates are only available every five years, we track progress for this target annually using mortality rates.
From 1998 to 2014, the overall Indigenous mortality rate has declined significantly (by 16 per cent) and there has been a significant decline in the gap (of 13 per cent) 29. Figure 11 shows the trajectory to the target and that the current rates are not on track. It also shows that mortality rates are continuing to decline for both populations.
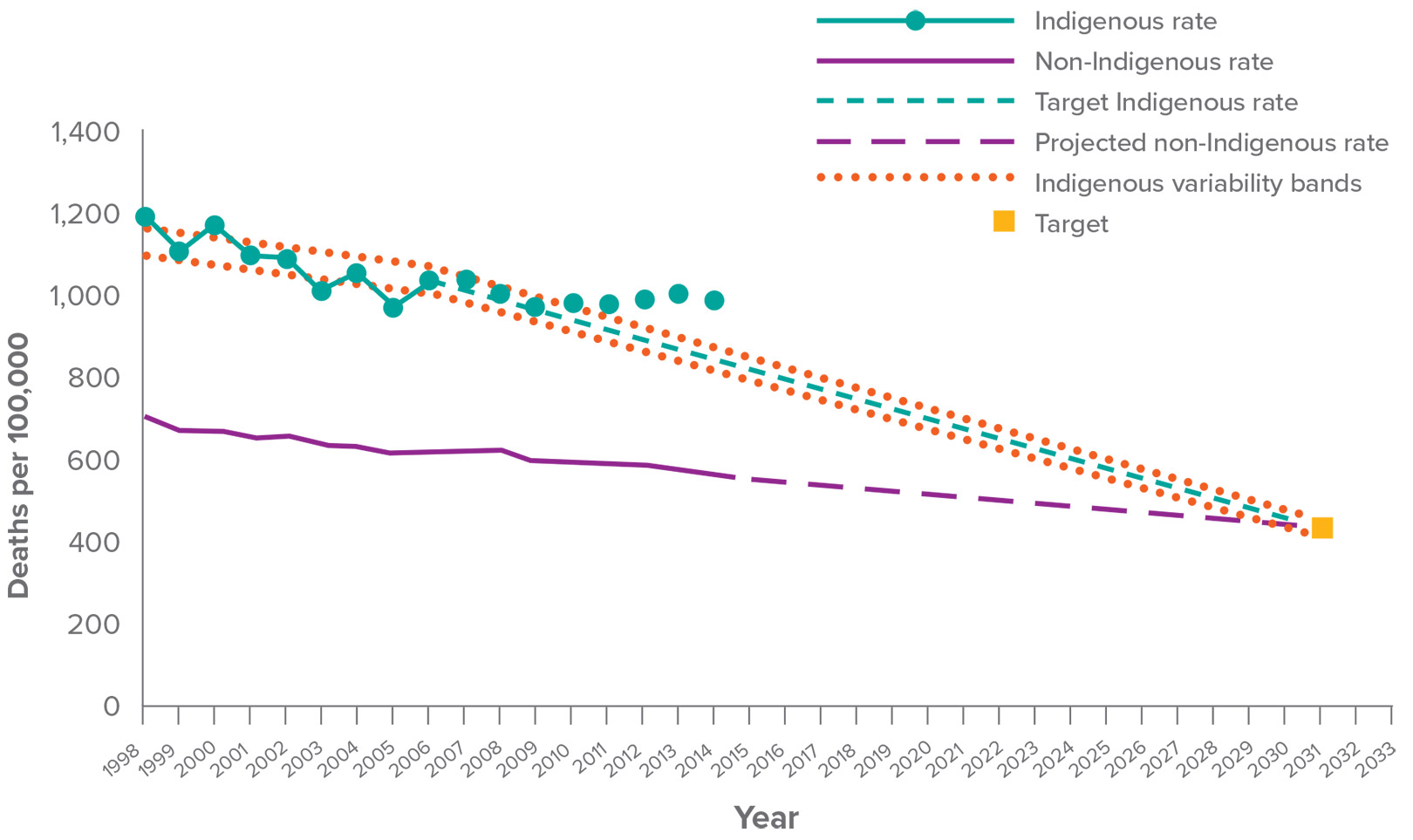 Source: ABS and AIHW analysis of National Mortality Database
Source: ABS and AIHW analysis of National Mortality Database
Health outcomes at a population level generally do not improve within short or medium timeframes. There is a time lag between interventions and improvements in outcomes. While it is undeniable that progress needs to be faster, there have been long-term, gradual improvements in health outcomes.
Over the long-term, improvements in health care access and reductions in smoking are expected to have a positive impact. From 2002 to 2012-13, there has been a 7 percentage point decline in smoking rates for Aboriginal and Torres Strait Islander people aged 15 years and over (from 51 per cent to 44 per cent). Over the same period, for those who continue to smoke, there has also been a decline in the average number of cigarettes smoked daily. Despite these improvements, in 2012-13 Aboriginal and Torres Strait Islander people aged 15 years and over were still 2.5 times as likely to be a current smoker as non-Indigenous Australians.
Chronic disease accounts for around three quarters of the gap in mortality rates between Indigenous and non-Indigenous Australians. Between 1998 and 2013, the Indigenous mortality rate from circulatory disease decreased by 41 per cent and the gap has narrowed. Over the same period there was also a significant decline in the Indigenous mortality rate from respiratory disease (by 27 per cent). Between 2006 and 2013 there was a significant decline in the Indigenous kidney disease mortality rate (by 38 per cent).
However, cancer mortality rates are rising and the gap between Indigenous and non-Indigenous Australians dying from cancer is widening. Between 2006 and 2013, there was a 10 per cent increase in cancer death rates for Indigenous patients and a 6 per cent decline for non-Indigenous Australians.
Australia remains on track to eliminate trachoma from remote Aboriginal communities by 2020. The 2014 Australian Trachoma Surveillance Report (National Trachoma Surveillance and Reporting Unit, 2015) shows the overall prevalence of active trachoma in screened five to nine-year-olds decreased from 14 per cent in 2009 to 4.7 per cent in 2014.
case study Birthing in Our Communities
In Brisbane, improving the continuity of services and making them more culturally responsive to the needs of Aboriginal and Torres Strait Islander women and their families is producing encouraging results. With Australian Government funding, the Institute for Urban Indigenous Health, the Brisbane Aboriginal and Torres Strait Islander Community Health Service and the Mater Hospital have partnered to offer a midwifery group practice model of maternity care. In its first two years 197 Aboriginal and Torres Strait Islander women participated in the programme. Over that period:
- 76 per cent of women attended for their first antenatal visit in the first trimester of pregnancy, with 88 per cent attending for at least five visits during the antenatal period.
- Smoking rates among pregnant women decreased from 36 per cent at the first antennal visit to 24 per cent at the time of discharge from the Birthing in Our Communities programme.
- Only 17 per cent of women required delivery by caesarean (compared to 32 per cent nationally).
- Rates of both preterm birth and low birth weight were as low as 6 per cent, around half the national rates of both measures for Aboriginal and Torres Strait Islander babies, with only 7 per cent of infants requiring admission to the neonatal nursery.
- At the time of discharge from the Birthing in Our Communities programme, 81 per cent of women were exclusively breastfeeding.
Looking beyond mortality rates, biomedical samples were collected for the first time as part of the 2012-13 Health Survey (ABS, 2014) 30. This biomedical data provides clinical measures of disease in addition to the data usually collected on self-reported conditions. Based on this data, 11 per cent of Indigenous adults had diabetes, which was three times the non-Indigenous rate. The survey also tested for signs of kidney disease, with 18 per cent of Aboriginal and Torres Strait Islander people showing signs of kidney problems. Almost 90 per cent of those showing signs of kidney disease did not have a diagnosed condition.

Implementation Plan for the National Aboriginal and Torres Strait Islander Health Plan
Kidney disease if left untreated can result in kidney failure, or end stage kidney disease requiring regular dialysis treatment. Rates of Indigenous Australians commencing treatment for end stage kidney disease are much higher in remote areas (over four times as high) compared with rates in major cities.
Accelerating progress
To meet the life expectancy target, Aboriginal and Torres Strait Islander life expectancy must increase at a faster rate than the general population. There is a long lead time before changes in the health system and in people’s lives start to impact on life expectancy. The Australian and state and territory governments and Aboriginal community controlled health services all play a role in the delivery of prevention, primary care and acute care services.
Collaboration across governments, the health sector and Aboriginal and Torres Strait Islander people underpins the Implementation Plan for the National Aboriginal and Torres Strait Islander Health Plan 2013-2023. Recognising the centrality of culture in the health of Indigenous Australians, the Implementation Plan has a strong focus on prevention as well as supporting local and regional responses to identified needs.
Collaboration was key in developing the Implementation Plan. Indigenous leaders from the health sector, who make up the National Health Leadership Forum (NHLF), partnered with the Australian Government to inform the development. They will continue to monitor and review the implementation of actions, ensuring ongoing involvement of Aboriginal and Torres Strait Islander stakeholders.
To maintain efforts to improve health outcomes, including chronic disease prevention and management, the Australian Government funds Indigenous-specific and mainstream programmes including:
- $3.3 billion over four years from 2015-16 for primary health care and supporting infrastructure through the Indigenous Australians’ Health Programme – an increase of over $500 million compared to the previous four years. This includes $94 million for expanded maternal and child health programmes and $116 million for a targeted Tackling Indigenous Smoking programme.
- $85 million over three years from July 2016 to improve access to culturally sensitive, integrated mental health services for Aboriginal and Torres Strait Islander people, commissioned at the local level by Primary Health Networks (PHNs), with the close involvement of Aboriginal community controlled health services.
- $241 million over four years from July 2016 for local alcohol and drug treatment services in response to the National Ice Taskforce’s Final Report, including a substantial investment in local Aboriginal and Torres Strait Islander services through PHNs, with the close involvement of Aboriginal community controlled health services.
- Medicare Benefits Schedule – between July 2009 and June 2014, Indigenous health assessment rates for 0 to 14-year-olds increased by 184 per cent; 15 to 54-year-olds increased by 204 per cent; 55 and over increased by 156 per cent (Figure 12). In the same period, GP management plans and team care agreements claimed by Aboriginal and Torres Strait Islander people have doubled. Rates are now higher for these services for Indigenous Australians than non-Indigenous Australians.
- Pharmaceutical Benefits Scheme – between 1 July 2010 and 30 June 2015, more than 345,000 Aboriginal and Torres Strait Islander Australians have received assistance with the cost of medicines for chronic disease.
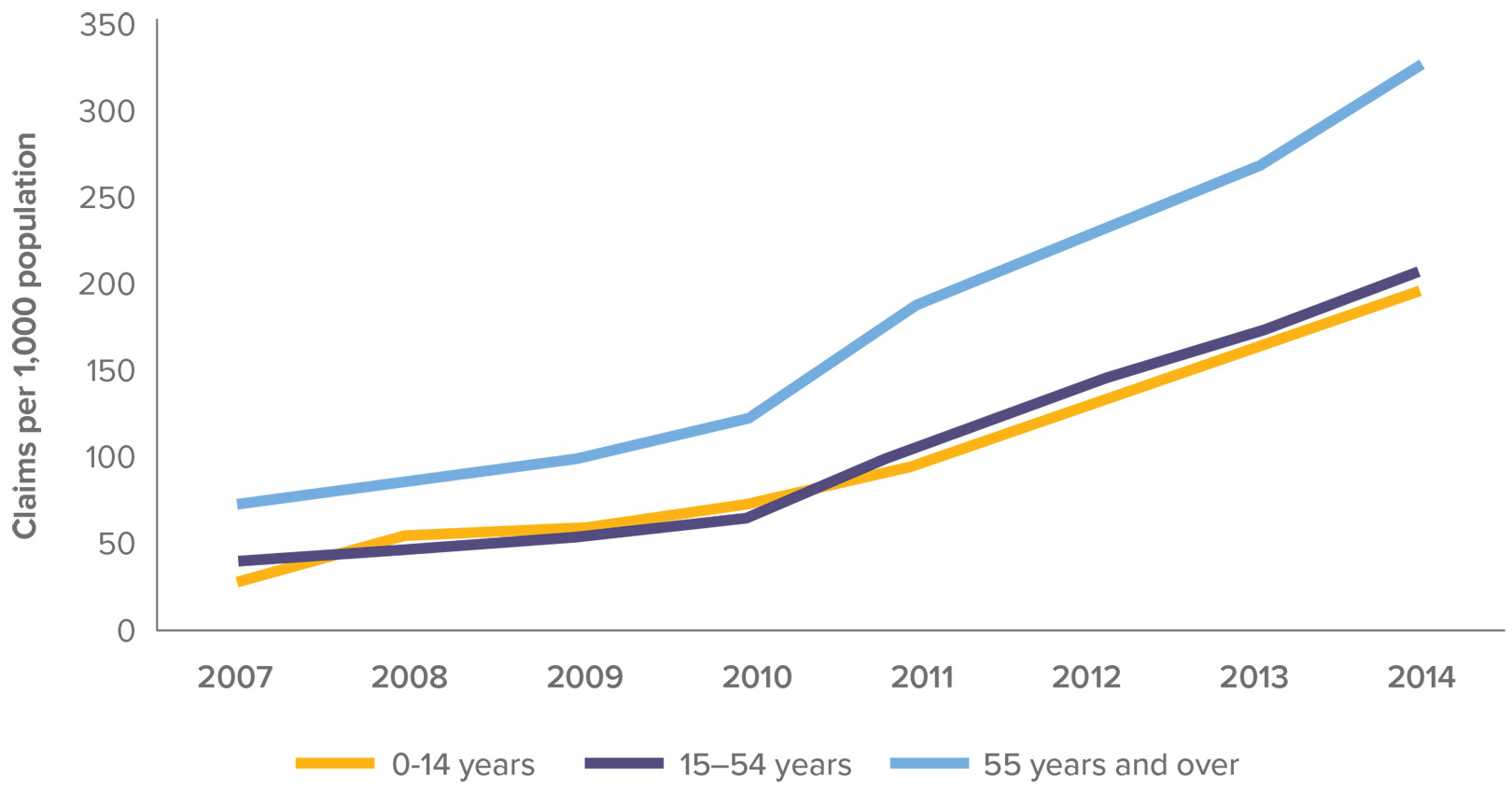 Source: AIHW analysis of Medicare Australia data
Source: AIHW analysis of Medicare Australia data

Dr Nadeem Siddiqui, Executive Director, Clinical Services treating Greg Hazel at the Winnunga Nimmityjah (Strong Health) Aboriginal Health Service, Australian Capital Territory
Health workforce
The Aboriginal and Torres Strait Islander workforce is integral to ensuring the health system addresses the needs of Indigenous Australians. They can improve patient care, access to services and ensure culturally appropriate services. There has been an increase in the proportion of the Indigenous population employed in health-related occupations from 1 per cent of the Indigenous population in 1996 to 1.6 per cent in 2011. However, this is still below the proportion of the non-Indigenous population employed in health-related occupations (3.4 per cent).
The Greater Northern Australian Regional Training Network aims to improve the capacity of the Aboriginal and Torres Strait health workforce:
- Aboriginal Health Worker/Practitioners Training Pathway model enhances clinical training and placement capacity for Aboriginal Health Workers in rural and remote Aboriginal community controlled health services.
- Northern Australia Indigenous Health Workforce Network identifies clinical placement capacity within Aboriginal health and develops the Indigenous health workforce.
case study Wiradjuri woman Ekala French is working hard to close the health gap

Wiradjuri woman Ekala French is passionate about improving Indigenous health.
Ekala, a Wiradjuri woman from central New South Wales, is an Aboriginal Health Worker with the Orange Aboriginal Medical Service. After finishing high school Ekala began a traineeship, working to address the health issues affecting Aboriginal people in the Orange region. This included working on a population health approach in the area to address the health of the whole community rather than just the individual. “By looking at the health issues facing a community, we can better identify the gaps in the services offered and how we can improve our services, particularly in primary health prevention,” Ekala said.
Ekala is already planning the next step of her career in Indigenous health, “I have a passion about Aboriginal health and I’m looking to become a nurse. Health workers are important to a community’s wellbeing but as a nurse I’ll have a greater opportunity to work with my community and offer services health workers can’t provide.”
Mental Health and Social and Emotional Wellbeing
Recognising Aboriginal and Torres Strait Islander people experience higher rates of mental health issues than other Australians and as part of its response to Contributing Lives, Thriving Communities – Review of Mental Health Programmes and Services, the Government is providing $85 million over three years, from 1 July 2016, to improve access to culturally sensitive, integrated mental health service
Under this initiative, Primary Health Networks will plan, commission and implement services joining up closely related services for Aboriginal and Torres Strait Islander mental health, social and emotional wellbeing, suicide prevention and alcohol and other drug treatment. Primary Health Networks in each region will lead the reform work, and collaborate closely with relevant local Indigenous and mainstream primary health care organisations, including Aboriginal community controlled health services and peak bodies.
In 2015-16 more than $38 million under the Indigenous Advancement Strategy: Community Safety and Wellbeing Programme is being invested in programmes aimed at boosting the resilience of Aboriginal and Torres Strait Islander people and their capacity to respond to stressors in their lives. Services include counselling, case management and healing activities. Seven Link-Up services across Australia offer emotional support to members of the Stolen Generations as they access personal and family records and arrange family reunions.
case study Preventing Youth Suicide
Around Australia, Indigenous youth and young adult suicide is high: from 2008–2012, the suicide rate for Indigenous Australians was almost twice that of non-Indigenous Australians. Of particular concern is the rate for Indigenous males aged 20-24 years.
But psychologist Tanja Hirvonen believes there is hope. An Aboriginal woman who grew up in Mount Isa, Tanja is one of 60 Aboriginal and Torres Strait Islander psychologists who are members of the Australian Indigenous Psychologists Association (AIPA).
She says the number of people lost to suicide is devastating.
“There is immeasurable loss which extends across our immediate and extended families, kinship networks and peer groups, communities and states.
“Suicide is a complex issue and there’s no one specific reason why someone might end their life. What we do know though is that chronic life stressors such as poverty, lack of education, high levels of substance use and unemployment, which leads to elevated levels of psychological distress, are reported factors for increasing risks for suicide. As are issues like trauma and ongoing grief, and increased incarceration rates, along with loss of cultural identity,” she said.
But Tanja is optimistic about the early intervention and prevention programmes being developed and run by professionals and community members. “Evidence shows community-led solutions are the most effective. Cultural connections are known to be a key protective factor for robust social and emotional wellbeing. Connections to land, sea, country, family, community and spirituality are key. We need to work together nationally on this but each community will have its own response that will work best for them.”
Disability
There is a clear relationship between education, employment and disability. Indigenous adults with a profound, severe or moderate core activity limitation were less likely to have completed Year 12 compared to those without a disability (22 per cent compared with 33 per cent) (Figure 13).
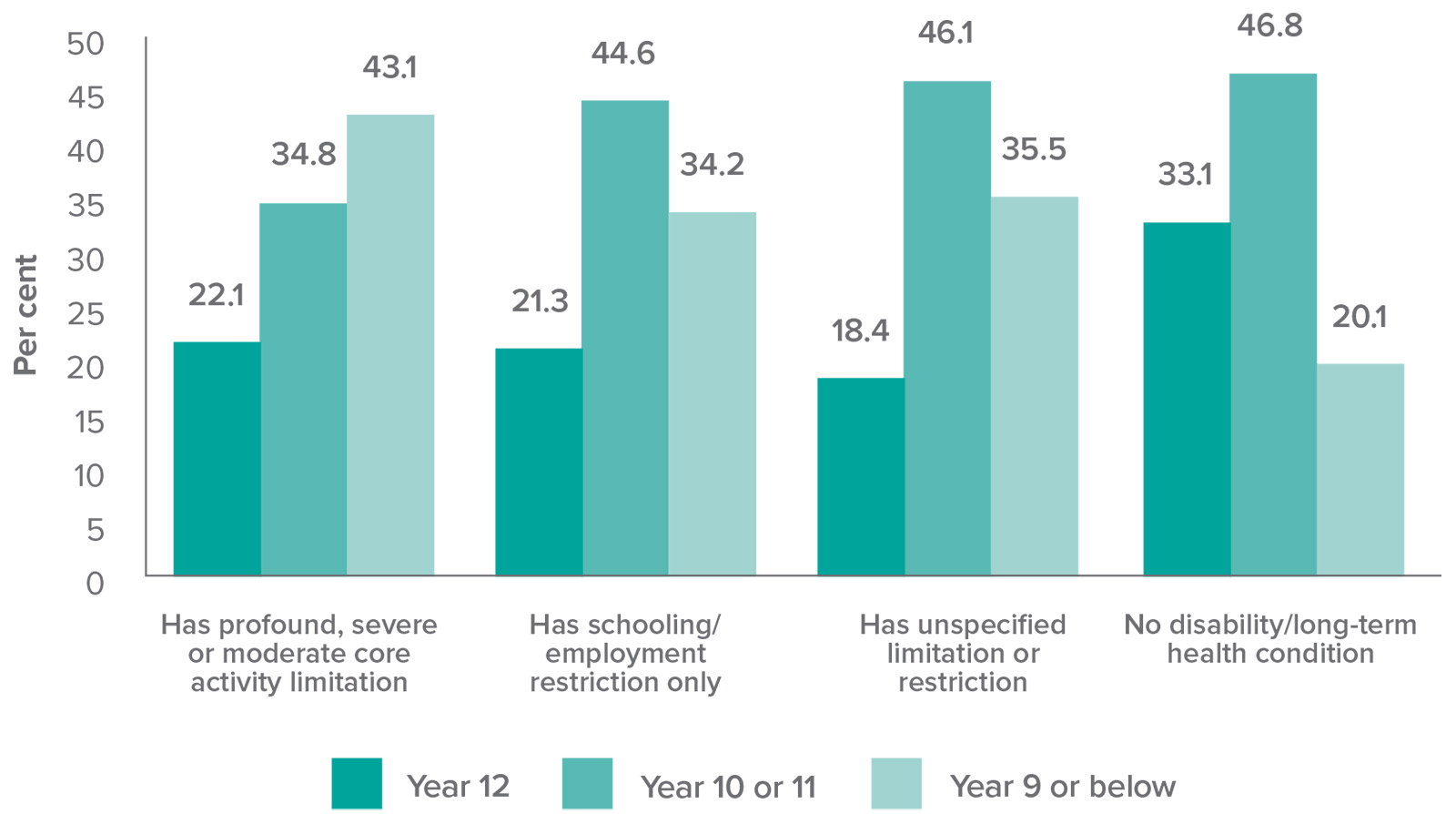 Source: ABS Australian Aboriginal and Torres Strait Islander Health Survey 2012-13.
Source: ABS Australian Aboriginal and Torres Strait Islander Health Survey 2012-13.
Disability has a large impact on Indigenous employment. Most Aboriginal and Torres Strait Islander people of workforce age without a disability were employed in 2012-13 (55.3 per cent). In contrast only 38 per cent of Aboriginal and Torres Strait Islander people with a disability were employed (Figure 14).
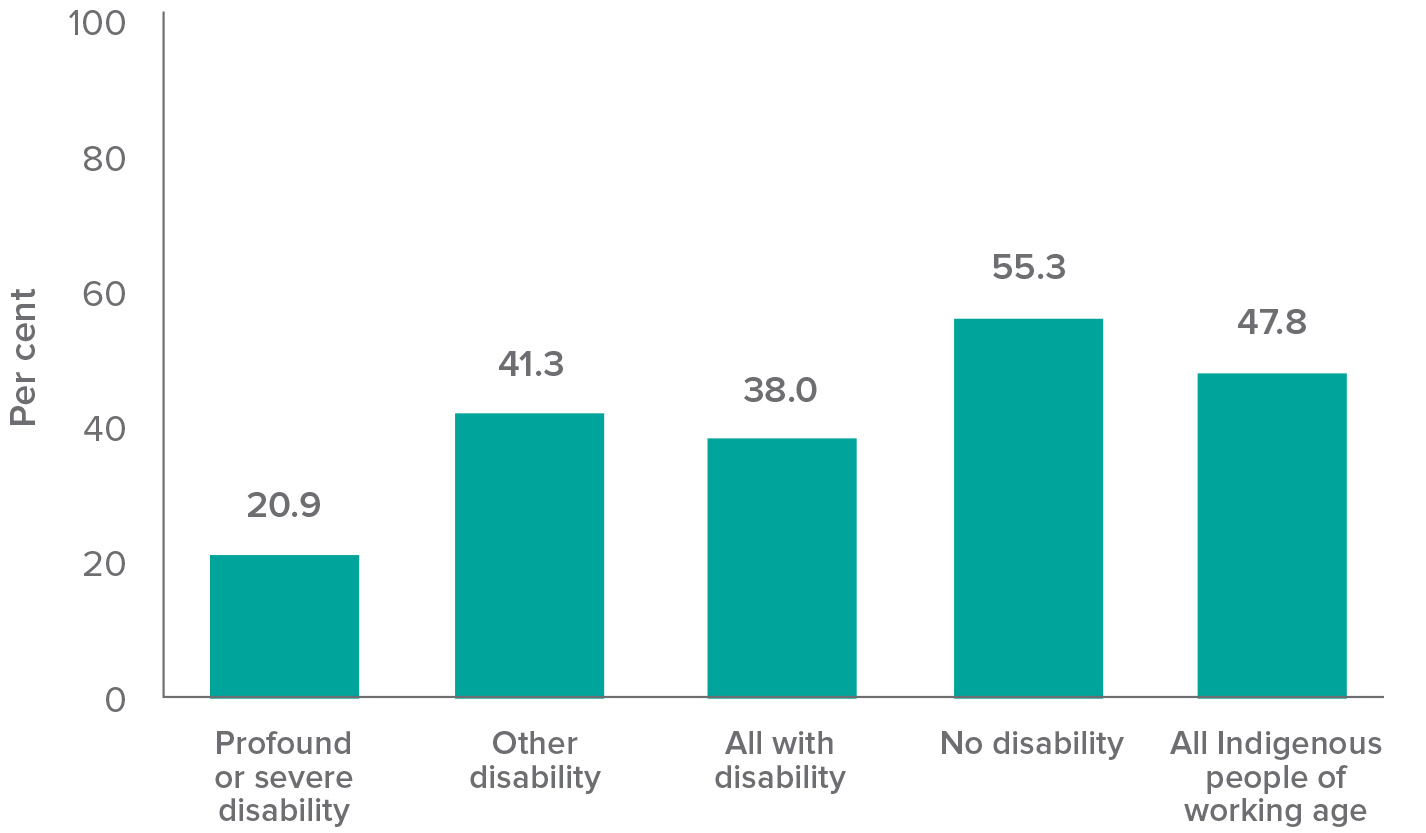 Source: ABS Australian Aboriginal and Torres Strait Islander Health Survey (NATSIHS component) 2012-13.
Source: ABS Australian Aboriginal and Torres Strait Islander Health Survey (NATSIHS component) 2012-13.
The National Disability Strategy provides a 10 year policy framework (2010 to 2020) to improve the lives of people with disability. The Strategy aims to improve the accessibility of mainstream services for people with disability and will complement existing specialist disability services and programmes. The introduction of the National Disability Insurance Scheme (NDIS) represents a significant action under the Strategy to support Aboriginal and Torres Strait Islander people access support across the lifespan:
- School Leaver Employment Supports project – aims to improve the pathway for young people with a disability from school to work through the collaborative effort of schools and Government employment services (in Tasmania and the ACT).
- Shared Support Plan project – explores the concept of integrating education and NDIS plans, focusing on opening communication pathways to ensure therapy strategies can be shared (in Barwon in Victoria).
- In the Barkly region of the Northern Territory, people with disability are receiving support including new equipment as part of a new community approach that builds local capacity through partnerships and is focused on developing solutions to the challenges of building the NDIS in remote and very remote areas.
Strategies are also in place to support people with disability into employment:
- Disability Employment Service – helping people with disability, injury or a health condition get ready to look for a job, find a job and keep a job. Four providers deliver specialist services for Aboriginal and Torres Strait Islander people from 21 sites in New South Wales, Queensland, Western Australia and South Australia. There is also financial assistance available for employers for workplace modifications, equipment and services.
- Supported Wage System – supports people whose work productivity is significantly reduced as a result of their disability.
case study Wheelchair basketballer Ryan Morich

National NAIDOC Sportsperson of the Year award winner and wheelchair basketballer player Ryan Morich.
Ryan Morich is a Noongar man from Western Australia, currently on a wheelchair basketball scholarship at the University of Alabama. He is the first Aboriginal person with disability to take up a sports scholarship in the USA.
In his first year, he made the Intercollegiate All-Rookie Team. In 2013, Ryan represented Australia at the Under 23 World Championships, where he led the team to a bronze medal win. He is currently a member of the Australian Rollers senior team. Ryan is captain of the Red Dust Heelers – a wheelchair basketball team with a strong focus on fostering future Aboriginal athletes with disability.
Ryan is partnered with the Wheeling and Healing Program, which helps people deal with negative feelings arising from their disability. He helps others by sharing his story on cancer, limb loss and losing loved ones to cancer. His goal is to represent his country at the Paralympic games and to further opportunities for young people with disability.
Veterans’ Affairs
The Indigenous Veterans’ Strategy 2015-2020 supports Aboriginal and Torres Strait Islander veterans and ex-serving personnel, and their families, to access repatriation benefits and entitlements. It sets out steps to develop and improve services within Indigenous communities. To improve its remote service delivery, the Department of Veterans’ Affairs delivers services via state and territory offices in partnership with government and non-government agencies.




