1.05 Circulatory disease
Page content
Why is it important?
Circulatory disease is a major cause of morbidity and mortality among Australians. Circulatory disease is more common among Indigenous Australians and tends to occur at much younger ages (Katzenellenbogen et al, 2014; Bradshaw et al, 2011; AIHW, 2015b; Brown, 2012). Risk factors such as physical inactivity, obesity, diabetes and high blood pressure are more prevalent among Indigenous Australians than non-Indigenous Australians (Gray, C et al, 2012). Smoking levels are high among Indigenous adults, although there has been a significant reduction in recent times (see measure 2.15). Low socio-economic status is associated both with greater risk of developing circulatory disease and with lower chance of receiving appropriate treatment (Beard et al, 2008; Cunningham, 2010).
Findings
Circulatory diseases were the third leading cause of disease burden for Indigenous Australians, representing 12% of the burden; and the leading cause of the health gap between Indigenous and non-Indigenous Australians in 2011 (19% of the gap) (AIHW, 2016f). There was a 21% reduction in the Indigenous burden from circulatory diseases between 2003 and 2011, with most of this improvement in fatal burden. This disease group was dominated by coronary heart disease (58%) and stroke (14%). Most circulatory burden for Indigenous Australians was due to early death (88%); predominantly in those aged 30 years and over; higher for males (58%) than females (42%).
In 2011–15, circulatory disease was the leading cause of death among Indigenous Australians (24% of deaths) with an age-standardised death rate 1.6 times that for non-Indigenous Australians. The leading causes of Indigenous circulatory disease deaths were ischaemic heart disease (55%), followed by cerebrovascular disease including stroke (17%). There has been a 43% decline in the Indigenous circulatory disease mortality rate between 1998 and 2015 and a significant narrowing of the gap between Indigenous and non-Indigenous Australians. A study in the NT found an increase in incidence of acute myocardial infarction and at the same time an improvement in survival both prior to and after hospital admission (You et al, 2009). Studies in the NT also showed survival for stroke has improved among both non-Indigenous and Indigenous Australians over time (from 1999-2011 in (You et al, 2015); and from 1992 to 2013 in (Zhao et al, 2015a)). However, the incidence rate has not changed for both non-Indigenous and Indigenous Australians in the NT from 1999 to 2011 (You et al, 2015).
Based on self-reported data from the 2012–13 Health Survey, 13% of Indigenous Australians had a circulatory condition. This is a significant increase from 11% in 2001. Rates increased with age and 23% of those aged 25 years and over reported the condition. After adjusting for differences in the age structure of the two populations, Indigenous Australians were 1.2 times as likely to report having circulatory disease as non-Indigenous Australians. The greatest disparities were in the 25–54 year age groups. This disease was more common in Indigenous women (14%) than men (11%). Indigenous Australians living in remote areas reported higher rates of circulatory disease than those in non-remote areas (18% compared with 11%). Around 45% of Indigenous Australians aged 15 years and over reporting diabetes (and 47% of those reporting kidney disease) also reported having circulatory diseases. Indigenous Australians were also more likely to report having circulatory disease if they lived in the most disadvantaged areas (20%) compared with the most advantaged areas (10%) (based on SEIFA); and if they completed schooling to Year 9 (27%) compared with those who completed Year 12 (12%). Indigenous adults who were obese had higher rates (26%) than those who were not obese (14%).
Based on GP survey data (2010–15), around 8% of problems managed by GPs for Indigenous patients related to circulatory conditions. After adjusting for differences in the age profile of the two populations, Indigenous patients were managed for hypertension at a similar rate to other Australians; while rates for managing heart failure and ischaemic heart disease were 74% and 55% higher respectively. Indigenous patients were half as likely to receive cardiac check-ups at GP encounters as other Australians.
For the two years to June 2015 the circulatory disease hospitalisation rate for Indigenous Australians was 1.8 times that for non-Indigenous Australians (after adjusting for age). Indigenous Australians had higher rates of hospitalisation for circulatory disease across all age-groups. Hospitalisation rates were higher for Indigenous males (18 per 1,000) than Indigenous females (16 per 1,000).
Since 2004–05, there has been a 17% increase in the Indigenous hospitalisation rate for circulatory disease and a 12% decline for non-Indigenous Australians (in NSW, Vic, Qld, WA, SA and the NT combined). Ischaemic heart disease was the most common type of circulatory disease resulting in hospitalisation for Indigenous Australians (39%) followed by pulmonary and other heart diseases (33%). Diabetes and kidney disease were common comorbidities. Hospitalisation rates for Indigenous Australians were 7.3 times the rate for other Australians when all three diseases are present (AIHW, 2014g).
Indigenous Australians hospitalised for coronary heart diseases were around half as likely to receive coronary angiography (0.7 times) and revascularisation procedures (0.6 times) (see measure 3.06). The proportion of Indigenous Australians hospitalised for a heart attack that received an angiography or revascularisation procedure increased from 32% in 2004–05 to 50% in 2013–14. However, this was still lower than for non-Indigenous Australians (63%) (AIHW, 2016a). According to one study in the NT, Indigenous Australians were less likely to receive in-patient cardiac rehabilitation, prescription of statins on discharge, and were more likely to die in the two years after discharge (Brown, 2010). Randall et al. (2013) reported that over the period 2000 to 2008, Indigenous Australians in NSW had a 37% lower rate of revascularisation in the 30 days after admission with myocardial infarction compared with non-Indigenous Australians. This disparity was largely explained by the hospital of admission (hospitals in rural areas had lower revascularisation rates for all patients), a higher comorbidity burden and lower rates of private health insurance. Patients admitted to smaller more remote hospitals without onsite angiography had increased risk of short-term and long-term mortality (Randall et al, 2012). A recent study in WA also found gaps in access to cardiac rehabilitation and secondary prevention services for Indigenous Australians (Hamilton et al, 2016).
Figures
Figure 1.05-1
Self-reported circulatory disease, Indigenous persons (2 years and over), by jurisdiction and remoteness, 2012–13
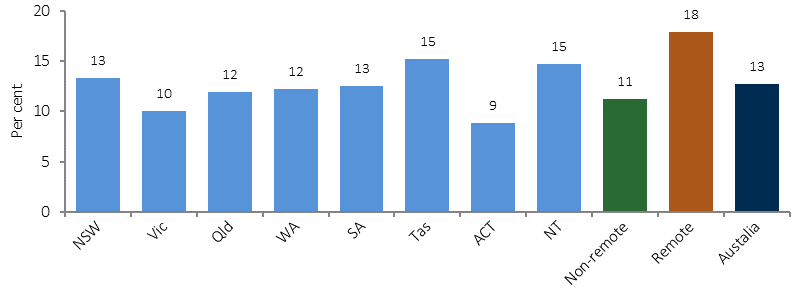
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Figure 1.05-2
Self-reported heart and circulatory disease, by age and Indigenous status, 2012–13
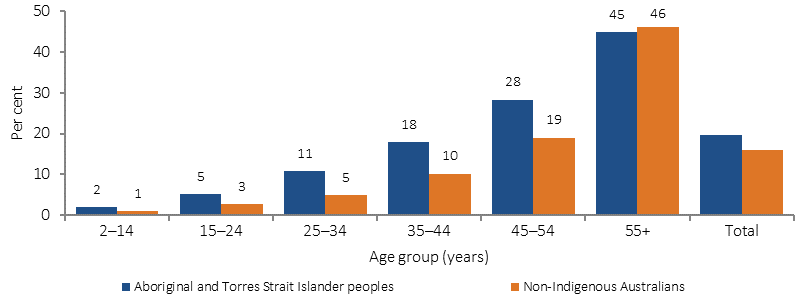
Note: Total is for people aged 2 years and over and is age standardised
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Figure 1.05-3
Age-standardised death rates for circulatory disease, by Indigenous status, 1998 to 2015
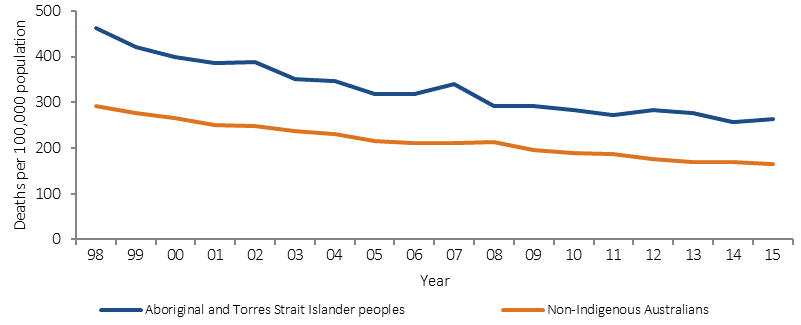
Source: ABS and AIHW analysis of National Mortality Database
Figure 1.05-4
Age-specific hospitalisation rates for circulatory disease, by Indigenous status, July 2013–June 2015
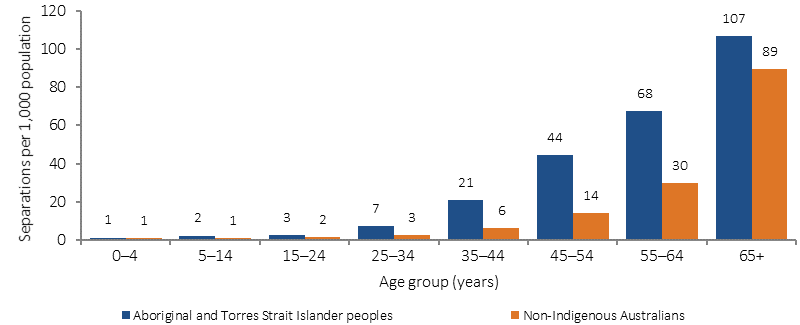
Source: AIHW analysis of National Hospital Morbidity Database
Implications
In recent decades, Australian mortality rates from circulatory disease have fallen, due to reduced smoking; improved management of high blood pressure and heart disease; and improved treatments for heart attack and stroke. However, high rates of obesity and diabetes threaten to slow or reverse these improvements. Circulatory disease problems were managed by GPs at similar rates for Indigenous Australians and other Australians. A recent study in Australian primary health care centres showed the importance of raising awareness and assessment of risk factors in young Indigenous people and implementing preventive health care strategies (Crinall et al, 2016). Hospitalisation rates for circulatory disease were higher among Indigenous Australians but, despite improvements, they were still less likely to receive coronary procedures when in hospital than non-Indigenous Australians. This may be due to Indigenous patients facing health care providers who lack cultural competency training, so improvements are required (NHF & AHHA, 2010). A study in the NT of avoidable mortality for Indigenous Australians between 1985 and 2004 found improvements in conditions amenable to medical care but marginal improvement for conditions responsive to preventative measures. The study noted the reduction of deaths from stroke was consistent with improved drug therapies and intensive care, dedicated stroke units and surgical procedures (Li, SQ et al, 2009).
The Indigenous Australians' Health Programme (IAHP) focuses on the prevention, early detection and management of chronic disease through expanded access to and coordination of comprehensive primary health care. Activities aimed at helping patients who experience circulatory disease include Tackling Indigenous Smoking and a care coordination and outreach workforce based in AMSs and mainstream services. In addition, GP health assessments for Indigenous Australians are funded under the MBS, which includes follow-on care. Funding is also provided for incentive payments for improved chronic disease management, and for cheaper medicines through the PBS.
The Lighthouse Hospital Project, funded through the IAHP, aims to drive systemic change in the acute care sector to improve care and outcomes for Indigenous Australians who experience acute coronary syndrome. It is designed to improve governance, clinical quality, and cultural competence of the health workforce.
The National Recommendations from the May 2014 Better Cardiac Care for Aboriginal and Torres Strait Islander People Post-Forum Report focus on five priority areas for action by all jurisdictions, including: early cardiovascular risk assessment and management; early diagnosis of heart disease and heart failure; guideline-based therapy for acute coronary syndrome; the provision of ongoing preventive care; and strengthening the diagnosis, notification and follow-up of rheumatic heart disease. The second Better Cardiac Care report shows progress against 11 of the 21 recommended indicators, for which updated data were available (AIHW, 2016a).