2.16 Risky alcohol consumption
Page content
Why is it important?
Excessive consumption of alcohol is associated with health and social problems in all populations. Long-term excessive alcohol consumption is a major risk factor for conditions such as liver disease, pancreatitis, heart disease, stroke, diabetes, obesity and cancer. It is also linked to social and emotional wellbeing, mental health and other drug issues (NHMRC, 2009). Where mothers have consumed alcohol during pregnancy, babies may be born with Foetal Alcohol Spectrum Disorders (FASD) (Telethon Institute for Child Health Research, 2009).
Binge drinking contributes to injuries and death due to suicide, transport accidents, violence, burns and falls. For the general population, one-third of suicides for men and women and one-third of motor vehicle deaths for men have been linked to alcohol consumption (NHMRC, 2009). Alcohol abuse can also affect families and communities. It has the potential to lead to anti-social behaviour, violence, assault, imprisonment and family breakdown (NHMRC, 2009).
The 2011 Burden of Disease study estimated that alcohol harm accounts for 8% of the total burden of disease and injury for Indigenous Australians. Among the risk factors considered, alcohol was responsible for the greatest burden of disease and injury for Indigenous males aged 15–44 years and was also the leading cause for females aged 15–24 (AIHW, 2016f).
Findings
The National Health and Medical Research Council (NHMRC) states that ‘drinking no more than two standard drinks on any day reduces the lifetime risk of harm from alcohol-related disease or injury’ and that ‘drinking no more than four standard drinks on a single occasion reduces the risk of alcohol-related injury arising from that occasion’ (NHMRC, 2009).
The 2014–15 Social Survey collected self-reported data on those who exceeded the NHMRC lifetime and single occasion risk guidelines. Based on the survey, 40% of Indigenous Australians aged 15 years and over had abstained from alcohol in the previous 12 months.
Comparisons between Indigenous and non-Indigenous Australians are only available from the 2012–13 Health Survey. After adjusting for differences in the age structure of the two populations, Indigenous Australians were 1.6 times as likely to abstain from alcohol as non-Indigenous Australians.
In 2014–15, 31% of Indigenous Australians exceeded the single occasion guidelines (binge drinking) at least once in the last two weeks. Rates of binge drinking were higher for Indigenous males (41%) than females (22%), and were similar between remote and non-remote areas (41%). The binge drinking rate for Indigenous Australians declined significantly between 2008 and 2014–15 (from 38% to 31%), following a significant increase from the 2002 rate (35%).
In 2012–13, rates of binge drinking at least once per week were 20% in remote areas and 18% in non-remote areas.
In 2014–15, 15% of Indigenous Australians aged 15 years and over drank at levels that exceeded the NHMRC lifetime risk guidelines. There was a significant decline in lifetime risky drinking between 2008 and 2014–15 (from 19% to 15%).
In the 2012–13 Health Survey, Indigenous rates for exceeding the single occasion risk guidelines were 1.1 times the non-Indigenous rates, while for the lifetime risk there was no significant difference.
The 2012–13 Health Survey data, based on 24-hour recall, shows that the median amount of alcoholic beverages consumed was more than twice as high among Indigenous consumers (equivalent to 3 bottles of beer or 1.5 bottles of wine) than non-Indigenous consumers (equivalent to 1.2 bottles of beer or almost 5 glasses of wine). The median amount of alcoholic beverages consumed by Indigenous adults was higher in remote areas (1,717 grams) than non-remote areas (1,007 grams).
Excess alcohol consumption has significant impacts on communities. In 2014–15, 19% of Indigenous Australians aged 15 years and over reported experiencing a family stressor related to alcohol problems. The rate was higher in remote areas (23%) than non-remote areas (18%). One study in NSW found that, after controlling for social and demographic variables, rates of offensive behaviour and property damage tended to be higher in areas with higher levels of alcohol sales (Stevenson et al, 1999). There is a clear link between alcohol, violence and imprisonment (see measure 2.11).
Survey data provides an indication of the prevalence of alcohol consumption, but under-estimates actual consumption. Furthermore, it cannot be assumed that patterns of consumption are uniform across geographic regions (Stockwell et al, 2004). After considering a range of evidence, a review by Wilson and colleagues estimated the prevalence of harmful alcohol use in the Aboriginal and Torres Strait Islander population at twice that of the non-Indigenous population (Wilson, M et al, 2010).
Over the period 2011–15, in NSW, Qld, WA, SA and the NT combined, Indigenous males died from alcohol-related causes at 5 times the rate of non-Indigenous males, and Indigenous females at 6 times the non-Indigenous rate. Most deaths (300 out of 441 deaths) were due to alcoholic liver disease. Indigenous females were 7 times as likely as non-Indigenous females to have died from alcoholic liver disease. The age-standardised alcohol-related death rate among Indigenous Australians fell from 32 deaths per 100,000 in 1998 to 24 deaths per 100,000 in 2015 and the gap between Indigenous Australians and non-Indigenous Australians narrowed.
Over the period July 2013 to June 2015, there were 9,816 hospitalisations of Indigenous Australians with a principal diagnosis related to alcohol use. This represented 2% of all hospitalisations of Indigenous Australians (excluding dialysis). Rates were highest in remote areas (15 per 1,000) and lowest in inner regional areas (5 per 1,000). Indigenous males and females were hospitalised for diagnoses related to alcohol use at 4 times the rate of non-Indigenous males and females respectively. Acute intoxication was the most common reason Indigenous Australians were hospitalised for alcohol use (59%), followed by dependence syndrome (12%), alcoholic liver disease (10%), and withdrawal (10%). Indigenous Australians were hospitalised for acute intoxication at 11 times the rate of non-Indigenous Australians and for alcoholic liver disease at 6 times the rate. Between 2004–05 and 2014–15 hospitalisation rates relating to alcohol use increased for Indigenous females (5 to 7 per 1,000 population) and Indigenous males (10 to 11 per 1,000 population).
Figures
Figure 2.16-1
Alcohol risk levels by Indigenous status, persons aged 15 years and over, age-standardised, 2012–13
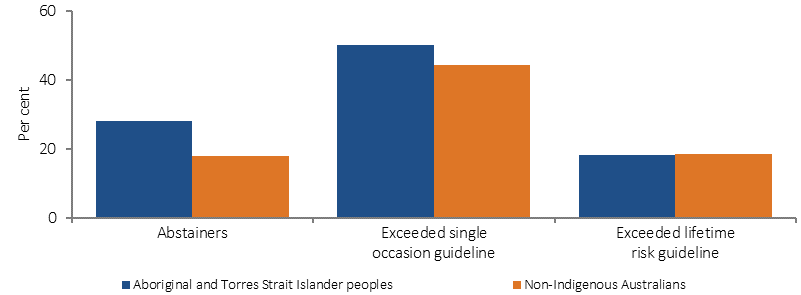
Note: Alcohol consumption levels are not comparable between the 2012–13 AATSIHS and 2014–15 NATSISS
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Figure 2.16-2
Indigenous Australians aged 15 years and over who exceeded single occasion risk guidelines, by remoteness area and sex, 2014–15
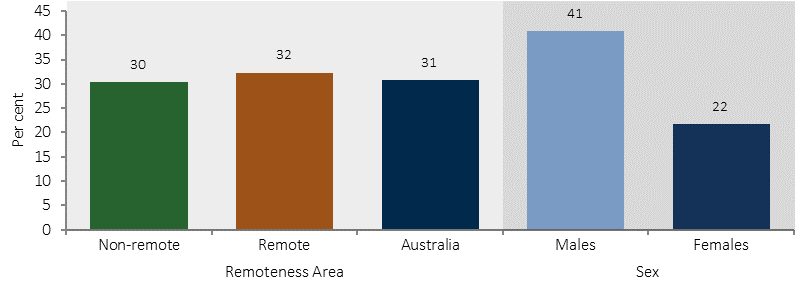
Source: ABS and AIHW analysis of 2014–15 NATSISS
Figure 2.16-3
Alcohol risk levels, Indigenous Australians aged 15 years and over, 2002, 2008 and 2014–15
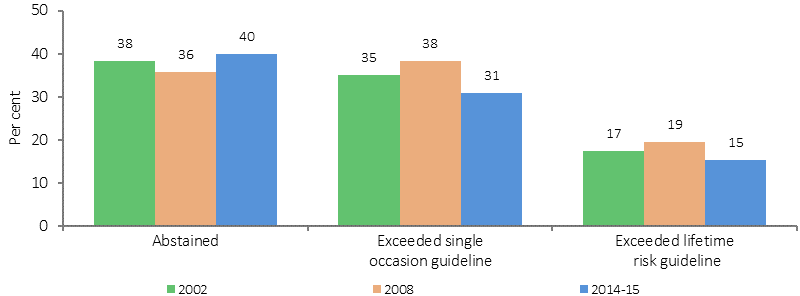
Source: ABS and AIHW analysis of 2002, 2008 and 2014–15 NATSISS
Figure 2.16-4
Age-standardised rates for deaths related to alcohol use, NSW, Qld, WA, SA and the NT, 2011–15
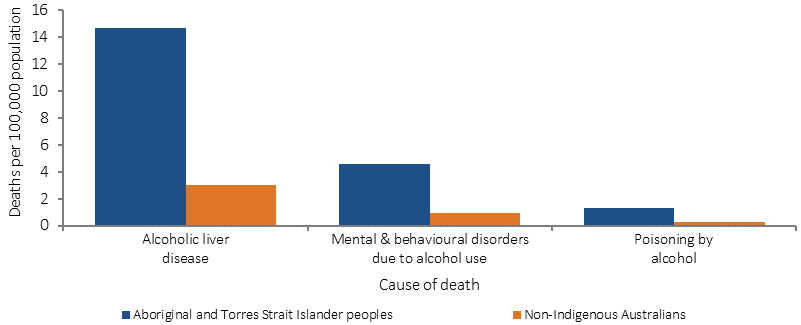
Source: ABS and AIHW analysis of National Mortality Database
Implications
The health effects of excess alcohol consumption are evident in both mortality and morbidity statistics. Reducing alcohol abuse can result in fewer assaults and less disability and improve the health and wellbeing of the population.
An evaluation of NSW ‘Lockout’ laws, including earlier cessation of alcohol, at venues in Sydney’s CBD and Kings Cross entertainment precincts found a subsequent reduction in assaults in Kings Cross (down 32%) and in the Sydney CBD (down 26%) (Menéndez et al, 2015). Reducing the number of alcohol sales outlets may also be effective, with a halving in the number of assaults in Aurukun attributed to the phased closure of the Aurukun tavern (Dept. of Social Services, 2012).
The National Drug Strategy (NDS) 2010–2015 provides the framework for an integrated and coordinated approach across all levels of government to reduce drug-related harm and drug use in Australia. The next NDS 2016–2025 is currently under development. The National Aboriginal and Torres Strait Islander Peoples Drug Strategy (NATSIPDS) 2014–2019 has been developed as a sub-strategy of the NDS 2010–2015. The goal of the strategy is to improve the health and wellbeing of Aboriginal and Torres Strait Islander people by preventing and reducing the harmful effects of alcohol and drugs on individuals, families, and their communities. The strategy has been informed by community consultation. In addition, a National Alcohol Strategy is currently being developed, and will complement the next NDS 2016–2025.
Australian Government funding for combatting alcohol and substance misuse includes support for a range of alcohol and other drug treatment services across Australia (see measure 3.11). Funding is provided through the Substance Misuse Service Delivery Grants Fund and Non-Government Organisation Treatment Grants Programme (administered by the Department of Health), Primary Health Networks, and the Indigenous Advancement Strategy—Safety and Wellbeing Programme (administered by the Department of the Prime Minister and Cabinet).
In addition, through the new National Partnership on Northern Territory Remote Aboriginal Investment the Australian Government is providing around $91.5 million (over 7 years) to tackle the harms caused by alcohol and other drugs in the Northern Territory.
On 25 June 2014, the Australian Government announced funding of $9.2 million for the National Fetal Alcohol Spectrum Disorders (FASD) Action Plan, which includes funding for Indigenous specific prevention and promotion activities. The FASD Action Plan is directed at the frontline of dealing with risky alcohol consumption—providing better diagnosis and management, developing best practice interventions, and services to support high-risk women. A review of 22 programmes in the US has found that pre-natal health screening followed by empathetic interventions by health professionals was effective in reducing alcohol use during pregnancy (AIHW & AIFS, 2014b).
Various strategies are in place in states/territories across Australia. For example, the Foetal alcohol spectrum disorder (FASD) prevention program is a project in the Kimberly region run by the Ord Valley Aboriginal Health Service. The programme applies innovative strategies in providing education and support of antenatal clients and their families, as well as education sessions to students in the region.
Strong Spirits, Strong Minds is a media campaign that aims to prevent and/or delay the early uptake of alcohol and other drugs by young Aboriginal people in the Perth metropolitan area, and was developed with input from an Aboriginal youth advisory panel. The project evaluation results indicate it is a highly effective and successful strategy (Holman & Joyce, 2014).