3.05 Chronic disease management
Page content
Why is it important?
Chronic diseases are the leading causes of illness, disability and death among Aboriginal and Torres Strait Islander peoples (see measures 1.02 and 1.23) and estimated to be responsible for 70% of the health gap (AIHW, 2016f).
Effective management of chronic disease can delay the progression of disease, improve quality of life, increase life expectancy, and decrease the need for high cost interventions leading to net savings (Thomas, SL, 2014; Zhao et al, 2014). It is therefore a key factor in meeting the target of closing the life expectancy gap between Indigenous and non-Indigenous Australians within a generation.
Good quality care for people with chronic disease often involves numerous health care providers across multiple settings and the engagement of the client and their family in self-management of the condition (NHPAC, 2006). Typically, the primary health care (PHC) provider plays a central role through: identifying patients with asymptomatic disease through systematic or opportunistic screening; developing a management plan with the patient and their family; regularly assessing the extent to which the chronic illness is controlled; conducting regular checks to identify early signs of complications; and referrals to specialist care where this is warranted.
Findings
The Medicare Benefits Schedule (MBS) includes items for GP management plans (GPMPs) and team care arrangements (TCAs) to support a structured approach to management of patients with chronic or terminal conditions. Between 2009–10 and 2015–16, the rate of claims by Indigenous Australians for TCAs increased (to 112 per 1,000), and was higher than the non-Indigenous rate (72 per 1,000). This is also the case for GPMPs (129 and 86 per 1,000). In 2015–16, for Indigenous Australians aged 15 years and over, there were around 59,500 claims for the preparation of a GPMP, 51,400 for coordination of TCAs, 48,300 for monitoring/supporting a person with a chronic disease care plan and 2,000 for Aboriginal Health Worker Services linked to Chronic Disease Management items. (see measure 3.18).
Commonwealth-funded Indigenous PHC organisations provide national Key Performance Indicators (nKPI) data on a range of process of care measures related to chronic disease management. In May 2015, around 32,900 regular clients of these organisations had Type 2 diabetes. Of these clients, 51% had a GPMP in the two years to May 2015 and 48% had a TCA. In the six months to May 2015, 52% of regular clients with Type 2 diabetes had their blood glucose levels tested, with 35% reporting a blood sugar result in the recommended range; 68% had their blood pressure assessed, with 43% reporting a result in the recommended range; and 67% had a kidney function test, with 81% reporting a result in the normal range.
In May 2015, of the 14,700 regular clients of Indigenous PHC organisations with cardiovascular disease, 63% had a kidney function test recorded; with 76% of those reporting a result in the normal range.
Indigenous PHC organisations also report on a range of services to manage chronic disease and provide continuity of care in the Online Services Report (OSR) (AIHW, 2016o). In 2014–15, of the 203 organisations, 77% employed a doctor, 96% kept track of clients needing follow-up, 84% had established relationships with Aboriginal liaison officers at the local hospital/s, 70% had shared care arrangements for chronic disease management, and 67% had well-coordinated discharge planning for Indigenous patients (e.g. provision of medicines, transport arrangements, liaison with GP and family).
In the 2012–13 Health Survey, 69% of Indigenous diabetics in non-remote areas reported having a blood test to check diabetes control in the previous 12 months and 68% had their feet checked compared with 72% and 74% respectively for non-Indigenous Australians. To manage their diabetes, 30% reported using insulin and 80% had taken lifestyle actions (diet, weight loss, and exercise).
Of those who knew they had diabetes, 61% had blood tests results indicating their diabetes was not well managed (compared with 44% for non-Indigenous Australians). This was more common among Indigenous males (72%) than females (53%). Of those with circulatory conditions, 91% reported having their blood pressure checked and 68% their cholesterol checked in the previous 12 months compared with 94% and 76% respectively for non-Indigenous Australians.
A recent study of Indigenous Australians in remote NT found that higher levels of primary care utilisation for renal disease reduced avoidable hospitalisations by 82–85%, deaths by 72–75%, and years of life lost by 78–81%. For patients with ischaemic heart disease there was a reduction in avoidable hospitalisation of 63–78%, deaths 63–66% and years of life lost 69–73% (Zhao et al. 2014).
Figures
Figure 3.05-1
Age-standardised rates of selected GPMPs and TCAs claimed through Medicare by Indigenous status, 2005–06 to 2015–16
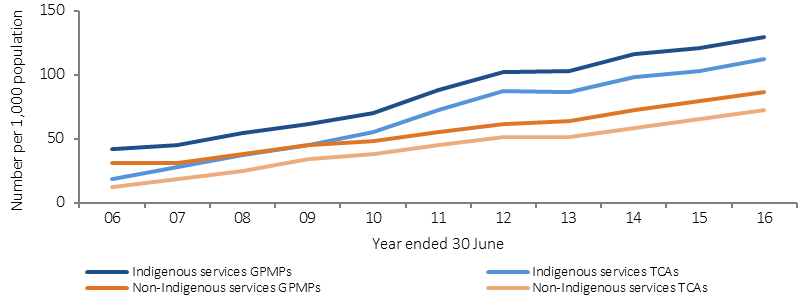
Source: Medical Benefits Division, Department of Health
Figure 3.05-2
Age-standardised rate of selected MBS services claimed, by Indigenous status, 2015–16
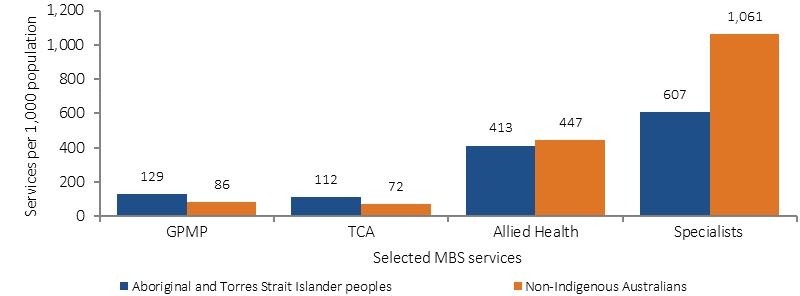
Source: Medical Benefits Division, Department of Health
Figure 3.05-3
Tests and results for regular clients with Type 2 diabetes, Commonwealth-funded Indigenous primary health care services, as at May 2015
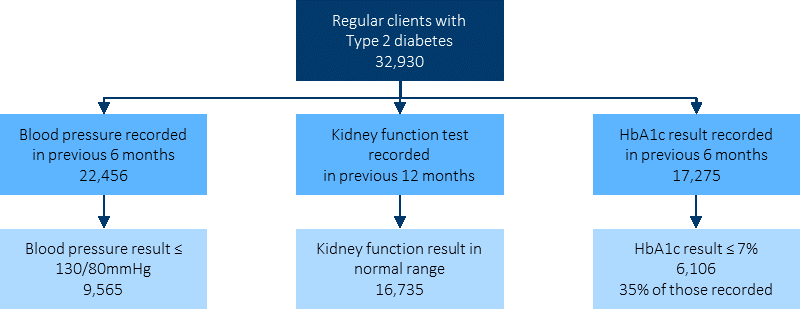
Source: AIHW analysis of national Key Performance Indicator data
Implications
Organised chronic disease management in primary health care services can lead to improved health outcomes (Hoy, W et al, 1999; Hoy, W et al, 2000; McDermott et al, 2003; Bailie, R et al, 2007; Zhao et al, 2014; Esterman et al, 2016; Harvey et al, 2013). For example, a 2014 study of chronic disease management in the NT found that even for people with the most complicated diabetes, regular attendance at their local health service for chronic disease checks reduced their risk of death significantly compared with those with newly diagnosed diabetes who rarely attend (Thomas, SL, 2014).
However, a range of studies have identified gaps and variation in the quality of chronic disease management in primary care settings for both Indigenous and non-Indigenous patients (Peiris et al, 2009; Webster et al, 2009; Schierhout et al, 2010; Panaretto et al, 2013).
Effective chronic disease care requires long-term strategies that promote and sustain engagement of Aboriginal and Torres Strait Islander people with health services (see measure 3.08). Strategies to support this include: flexible approaches that share decision-making and empower individuals to manage their conditions, strong local participation and connections with local communities, culturally appropriate education and health promotion, availability of Aboriginal Health Workers, and raising awareness in communities through education and health promotion (Bailie, RS et al, 2004; Bailie, C et al, 2016; Laycock & Brands, 2015).
For PHC services to play an effective role in chronic disease management, key features include: transparent work-practice systems backed by written disease management guidelines and manuals, appropriate staffing and training policies, delineated roles for all practitioner types, dedicated chronic disease management staff, intensive follow-up, established relationships with hospitals, specialists and allied healthcare workers, effective recall and reminder systems, connections with other services, patient-centred approaches, and participation in quality improvement processes (Panaretto et al, 2014; Wagner et al, 1996; Bodenheimer et al, 2002; Stoneman et al, 2014; Daws et al, 2014; Reilly et al, 2016; Sav et al, 2013).
Detailed descriptions of government initiatives to tackle chronic disease can be found in the Policies and Strategies section. These include the Indigenous Australians’ Health Programme (IAHP), which has a strong focus on prevention, early detection and management of chronic disease. Programmes include a care coordination and outreach workforce: Aboriginal Medical Services and mainstream services; and GP, specialist and allied health outreach services that support people living with chronic disease in urban, rural and remote communities.
The Australian Government also provides funding for GP health assessments for Aboriginal and Torres Strait Islander people under the MBS, including follow-up care. The Medicare Chronic Disease Management items, including GPMPs and TCAs, are used by doctors to plan and coordinate the care of patients who have chronic or terminal medical conditions. From 1 July 2017, the Health Care Homes initiative will roll out in selected PHNs. Eligible patients can enrol with a participating medical practice (‘home base’) for the ongoing coordination, management and support of their conditions.
The Practice Incentives Program—Indigenous Health Incentive (PIP–IHI) supports general practices and Indigenous health services to provide better health care for Indigenous patients, including best practice management of chronic disease. GPs receive payments for registering with the programme, for registering Indigenous patients with chronic disease and for providing best practice management of chronic disease.
The Medical Outreach Indigenous Chronic Disease Program aims to improve access to medical specialist, GP, allied and other health services for Aboriginal and Torres Strait Islander peoples. A total of $121.17 million from 2013–14 to 2016–17 has been committed for this measure.
The Quality Assurance for Aboriginal and Torres Strait Islander Medical Services program supports culturally appropriate and clinically effective management of diabetes patients in Indigenous communities. This occurs through training, technical support and quality assurance for ‘point of care’ pathology testing (e.g. HbA1c).
A National Strategic Framework for Chronic Conditions is being developed to provide guidance to all levels of government and health professionals to work towards the delivery of a more effective and coordinated national response to chronic conditions. The Framework moves away from a disease-specific approach recognising that there are often similar underlying principles for the prevention and management of many chronic conditions. It will better cater for shared health determinants, risk factors and multi-morbidities across a broad range of chronic conditions.