2.15 Tobacco use
Page content
Why is it important?
The health impact of smoking is evident in the high rates of hospitalisation and deaths from tobacco-related conditions (e.g. chronic lung disease, cardiovascular disease and many forms of cancer) (Marley et al, 2014; Pircher et al, 2012).
Maternal smoking during pregnancy increases the risk of poor outcomes for babies and children (see measures 2.21 and 1.01). Second hand smoke also has adverse health effects for those exposed to it (see measure 2.03).
In Australia, up to two-thirds of deaths in current smokers can be attributed to smoking and current smokers are estimated to die an average of 10 years earlier than non-smokers. Smoking cessation reduces mortality, with earlier cessation resulting in greater reductions (Banks et al, 2015).
It has been estimated that around 18,800 Australians die prematurely from tobacco-related diseases each year (AIHW, 2016l) and that smoking imposes an estimated $31.5 billion financial burden on the community (Collins & Lapsley, 2008).
Findings
Tobacco use was the leading contributor to the burden of disease among Indigenous Australians (12% of the total burden) and 23% of the gap in health outcomes between Indigenous and non-Indigenous Australians in 2011 (AIHW, 2016f). Coronary heart disease, COPD, lung cancer and stroke were key diseases attributable to tobacco use. Smoking caused 93% of the lung cancer burden and 87% of the COPD burden.
The 2014–15 Social Survey provides the latest data on Indigenous smoking rates. In 2014–15, 42% of Indigenous Australians aged 15 years and over reported being a current smoker (39% smoked daily and 3% less than daily). Indigenous Australians were 2.7 times as likely to be a current smoker as non-Indigenous Australians (age-standardised). The rate of current smokers among Indigenous adults (18 years and over) was 45% in 2014–15.
For Indigenous Australians aged 15 years and over, the rate of current smokers declined by 9 percentage points between 2002 and 2014–15. The short-term trend from 2008 to 2014–15 also declined (by 5 percentage points). Prior to 2002, rates were quite static. Over the same period, smoking rates for non-Indigenous Australians have also declined and there has been no improvement in the gap (24 percentage points in 2002 and 27 percentage points in 2014–15).
Indigenous Australians who lived in very remote areas were more likely to be current smokers in 2014–15 (53%) than those living in major cities (36%). This reflects the declines in smoking rates in non-remote areas (from 50% in 2002 to 39% in 2014–15). In remote areas, rates have remained steady (55% in 2002 and 52% in 2014–15). In 2014–15 Indigenous smoking rates ranged from 49% (in the NT) to 38% (Tas).
In 2014-15, smoking rates for Indigenous Australian males (45%) aged 15 years and over were slightly higher than for females (40%); and rates for both sexes have declined between 2002 and 2014–15. Smoking rates for Indigenous Australians aged 15 years and over were highest among those aged between 25 and 54 years (48–50%) and lowest for 15–17 year olds (17%); this pattern was similar for non-Indigenous Australians. Between 2002 and 2014–15, the greatest decreases in smoking rates have been in the younger age groups—from 58% to 41% for 18–24 year olds and from 33% to 17% among 15–17 year olds.
Consistent with the declining smoking rates for Indigenous Australians between 2002 and 2014–15, there has been an increase in the proportion of ex-smokers (from 15% to 22%). The proportion who had never smoked remained steady (33%–36%). For young people 15–17 years, the proportion who never smoked increased from 62% in 2002 to 78% in 2014–15 and for those aged 18–24 years, from 34% to 46%. This suggests a progressive decrease in the uptake of smoking. For those who continue to smoke, the average number of cigarettes smoked daily has declined from 15 in 2008 to 13 in 2014–15, noting there is no safe level of smoking.
In 2014–15, 69% of Indigenous daily smokers had tried to quit smoking in the previous 12 months. Rates were highest for those aged 25–34 years (77%). Rates of those who tried to quit and/or reduce smoking were higher for females (72%) than for males (67%). By remoteness and jurisdiction, there were differences for those who had tried to quit (not reduce) smoking—higher in remote than non-remote areas (43% compared with 25%) and higher in the NT (43%), WA (43%) and SA (36%) compared to other states and territories.
The most common reasons for trying to quit/reduce smoking in the previous 12 months were: general health (73%), cost (56%), improve fitness (31%), encouraged by family or friends (27%), medical advice (17%), and concerned about effect on others in the household (16%). In 2014–15, 59% of Indigenous Australians were living in a household with at least one smoker (See measure 2.03).
In a 2012–13 study (Thomas, DP et al, 2015a), 70% of Indigenous Australian smokers wanted to quit; 69% of daily smokers had ever made a quit attempt; 48% had made a quit attempt in the past year; and 47% of daily smokers who had made a quit attempt in the past 5 years had sustained an attempt for at least one month.
A 2017 study found the graphic warning labels on cigarette packaging appeared to have a positive impact on Indigenous smokers, who reported that it stopped them from having a smoke (Nicholson et al, 2017). Reasons for smoking appear to be similar for Indigenous men and women while motivations to quit differ (Knott et al, 2016). Predictors for making a quit attempt differ from predictors for sustaining a quit attempt (Nicholson et al, 2017). Predictors of smoking behaviour among adolescents differ for males and females (Mazanov & Byrne, 2008).
Smoking status is associated with socio-economic factors and smoking rates are highest for Indigenous Australians in the most disadvantaged circumstances (Thomas, DP et al, 2008). In NSW, tobacco outlet density has also been found to be higher in more disadvantaged districts and positively associated with smoking status (Marashi-Pour et al, 2015).
In 2014–15, Indigenous Australians aged 15 years and over were more likely to report being a non-smoker if they were: employed (65% compared with 47% for unemployed); in households in the highest income quintile (71% compared with 47% for the lowest); and had completed Year 12 (72% compared with 52% for those who completed Year 10 or below).
Indigenous Australians were more likely to report being a current smoker if they had: high/very high levels of psychological distress (51% compared with 38% for those with low/moderate levels); had fair/poor self-assessed health status (49% compared with 35% with excellent/very good); and had experienced one or more stressors in the previous 12 months (45% compared with 35% for those who did not).
Those who smoked were also more likely to drink at risky levels (42% exceeded short-term guidelines compared with 21% for non-smokers) and to use substances (44% compared with 21% for non-smokers). In 2015, 82% of Indigenous prison entrants were current smokers (see measure 2.11) (AIHW, 2015d).
Figures
Figure 2.15-1
Proportion of population aged 15 years and over reporting they are a current smoker, by Indigenous status and age, 2014–15
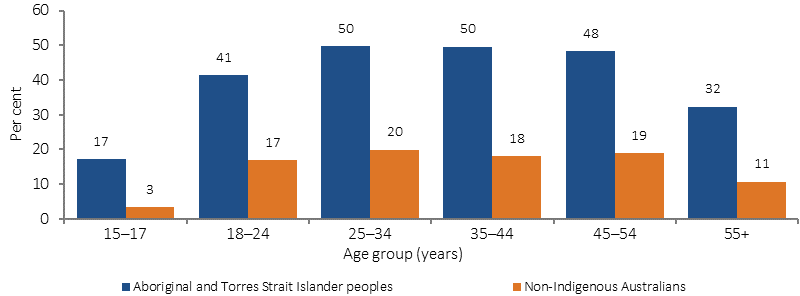
Source: ABS and AIHW analysis of 2014–15 NATSISS, 2014–15 NHS
Figure 2.15-2
Proportion of current smokers, Indigenous Australians aged 15 years and over, 2002, 2008, 2012–13 and 2014–15
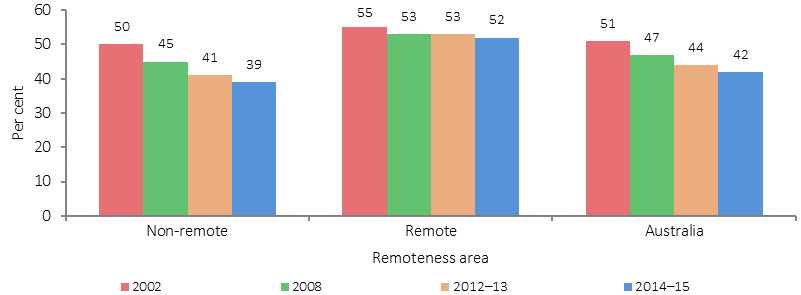
Source: ABS and AIHW analysis of the 1994 NATSIS, 2002, 2008 and 2014–15 NATSISS and 2012–13 AATSIHS
Figure 2.15-3
Smoker status, Indigenous Australians aged 15 years and over, 2002, 2008, 2012–13 and 2014–15
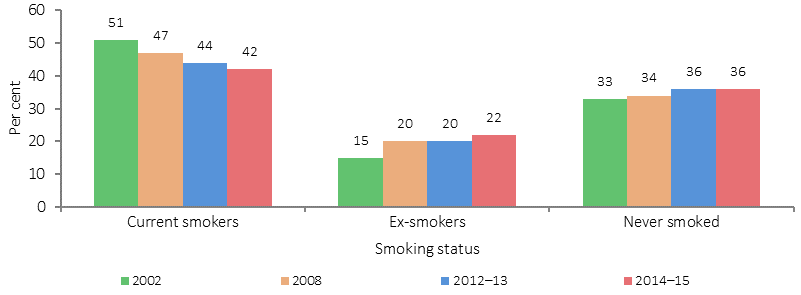
Source: ABS and AIHW analysis of the 1994 NATSIS, 2002, 2008 and 2014–15 NATSISS and 2012–13 AATSIHS
Table 2.15-1
Proportion of current smokers by age, sex, remoteness area and state/territory, Indigenous Australians aged 15 years and over, 1994, 2002, 2008, 2012–13 and 2014–15
| 1994 | 2002 | 2008 | 2012–13 | 2014–15 | |
|---|---|---|---|---|---|
| Age | |||||
| 15–17 | 30 | 33 | 22 | 19 | 17 |
| 18–24 | 56 | 58 | 53 | 46 | 41 |
| 25–34 | 63 | 58 | 56 | 54 | 50 |
| 35–44 | 57 | 58 | 53 | 50 | 50 |
| 45–54 | 49 | 49 | 48 | 48 | 48 |
| 55+ | 33 | 35 | 32 | 30 | 32 |
| Sex | |||||
| Male | 55 | 53 | 49 | 46 | 45 |
| Female | 49 | 50 | 45 | 42 | 39 |
| Persons | 52 | 51 | 47 | 44 | 42 |
| Remoteness area | |||||
| Major cities | 52 | 48 | 42 | 39 | 36 |
| Inner regional | 53 | 52 | 45 | 44 | 40 |
| Outer regional | 50 | 51 | 49 | 41 | 42 |
| Total non-remote | 51 | 50 | 45 | 41 | 39 |
| Remote | 54 | 53 | 50 | 49 | 51 |
| Very remote | 52 | 56 | 55 | 56 | 53 |
| Total remote | 53 | 55 | 53 | 53 | 52 |
| State/Territory | |||||
| NSW | 53 | 53 | 48 | 42 | 40 |
| Vic | 59 | 54 | 48 | 44 | 41 |
| Qld | 50 | 51 | 44 | 43 | 41 |
| WA | 51 | 48 | 44 | 43 | 46 |
| SA | 58 | 48 | 48 | 42 | 41 |
| Tas | 49 | 44 | 45 | 40 | 38 |
| ACT | 43 | 45 | 36 | 30 | 39 |
| NT | 50 | 56 | 53 | 54 | 49 |
| Australia | 52 | 51 | 47 | 44 | 42 |
Source: ABS and AIHW analysis of the 1994 NATSIS, 2002, 2008 and 2014–15 NATSISS and 2012–13 AATSIHS
Figure 2.15-4
Relationship between being a non-smoker and selected social factors, Indigenous Australians 15 years and over, 2014–15
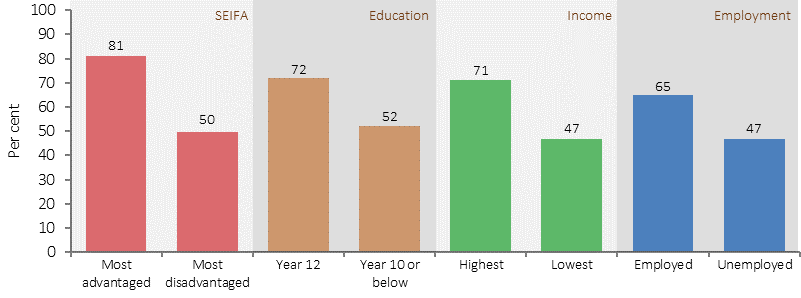
Source: ABS and AIHW analysis of the 2014–15 NATSISS
Figure 2.15-6
Smoking prevalence rates, people 15 years and over by Indigenous status and key tobacco control measures implemented in Australia since 1990
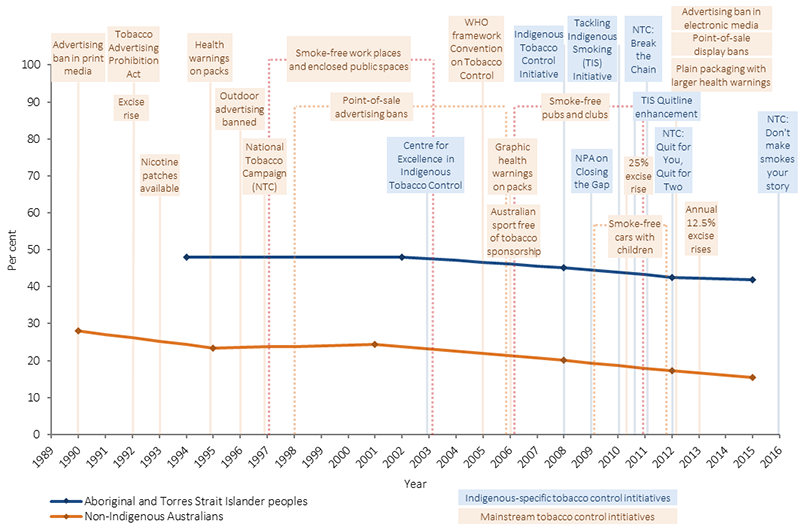
Sources: ABS and AIHW analysis of 1989–1990 National Health Survey (NHS), 1994 National Aboriginal and Torres Strait Islander Survey (NATSIS), 1995 NHS, 2001 NHS, 2002 National Aboriginal and Torres Strait Islander Social Survey (NATSISS), 2007–08 NHS, 2008 NATSISS, 2011–12 NHS (core), 2012–13 Australian Aboriginal and Torres Strait Islander Health Survey, 2014–15 NHS and 2014–15 NATSISS
Implications
Tobacco smoking is influenced by a range of social, cultural and family factors, including normalisation of smoking in peer groups and families, positive attitudes towards smoking, and smoking as a coping mechanism (Robertson et al, 2013; Scollo & Winstanley, 2012; Johnston & Thomas, 2008; Hearn et al, 2011). Additional barriers to quitting in remote areas include underlying social disadvantage and access to and uptake of services/treatment to support quitting (Thomas, DP et al, 2015a; Sarin et al, 2015).
The influence of these factors varies across the different community and social settings in which Aboriginal and Torres Strait Islander peoples live (Johnston & Thomas, 2008). Consequently, it is important that tobacco reduction strategies acknowledge the social exchange that occurs when smoking; the important role of family; and the high rates of stress experienced by Aboriginal people (Cosh et al, 2015; Hearn et al, 2011).
Systematic international reviews of smoking cessation intervention studies in Indigenous populations globally have found limited rigorous evidence to evaluate which interventions would be effective in reducing smoking; there is not one type of intervention or combination of activities that will reduce tobacco use in Indigenous communities (Carson et al, 2012; Minichiello et al, 2015).
What was found to have an important influence is a comprehensive approach inclusive of multiple activities (e.g. pharmacotherapies combined with culturally tailored interventions and health professional support); addressing prevention and cessation at the individual, community and legislative levels (e.g. brief interventions with community education and smoke-free policies); centred on Indigenous leadership; with long-term community investments; workforce support and development; and provision of culturally appropriate health materials and activities (Minichiello et al, 2015; Carson et al, 2012; Robertson et al, 2013; Hearn et al, 2011; Noble et al, 2016).
The research also highlighted that strategies should be evidence-based; coordinated; integrated (with each other, with mainstream smoking strategies and other Indigenous health strategies); involve Indigenous people; support, strengthen and build on existing programs; and further develop evidence (Sarin et al, 2015).
While comprehensive tobacco control programs appear to be motivating Indigenous Australians to quit, they do not appear to overcome the challenges in sustaining quit attempts, particularly for the more disadvantaged and those from remote areas (Nicholson et al, 2015).
Australian governments have worked closely with Indigenous Australians and health organisations over many years to deliver a range of approaches to address the high rates of tobacco smoking in the Indigenous population. Smoking rates are starting to decline; though are still high, particularly in remote areas. Further sustained improvements will be needed to close the gap in health outcomes.
The National Tobacco Strategy 2012–18 has nine priority areas; one building on existing programs and partnerships to reduce smoking rates among Aboriginal and Torres Strait Islander people. The Strategy includes demand reduction, supply reduction and harm reduction approaches (IGCD, 2012). A mid-point review of the Strategy (undertaken in 2016) assessed whether Australia is on track to meet the COAG targets to reduce smoking rates (see COAG targets).
Indigenous Australians are a major target audience of the National Tobacco Campaign (NTC). In 2016, Don’t Make Smokes Your Story, specifically targeting Indigenous smokers, was developed and placed in a range of Indigenous and mainstream media channels together with Break the Chain and Quit for You, Quit for Two (targeting pregnant women and their partners). The NTC encourages Indigenous smokers to quit smoking, and recent quitters to continue not to smoke and to encourage others to quit. The More Targeted Approach campaign (aimed at high-risk and hard-to-reach groups) also includes materials developed for Indigenous Australians. Evaluation research has found the NTC effectively promoted positive attitudes and intentions towards not smoking.
Since 1 December 2012, all tobacco products have been required to be sold in plain packaging with updated and expanded graphic health warnings. Annual 12.5% increases in excise on tobacco and tobacco-related products were implemented on 1 December 2013, and 1 September 2014, 2015 and 2016. The 2016–17 Budget includes a further four annual 12.5% increases in tobacco excise and excise equivalent customs duties to be implemented from 1 September 2017.
The Australian Government delivered the Tackling Indigenous Smoking (TIS) programme, commencing with funding for Tackling Smoking and Healthy Lifestyle Teams in 2010. Following a review in 2014, the TIS programme funds regional projects to deliver a range of evidence-based activities that suit the local context and the needs of the community to prevent the uptake of smoking and support smoking cessation. The regional projects have national supports to assist with best practice approaches and outcome measurement. Five nationally consistent performance indicators have been developed for organisations receiving TIS regional grant funding: quality and reach of community engagement; building capacity to support quitting; referrals to appropriate quitting support; supporting smoke-free environments; and appropriate engagement with relevant organisations involved in tobacco reduction in the region.
Jurisdictions are also implementing strategies to reduce smoking. For example, in WA, the Tackling Smoking–a development of Midwest Region Wide Tobacco Strategy and Campaign. This campaign used intervention approaches that included radio, newspaper, community events and the distribution of promotional materials. Results from a short-term evaluation indicated an increase in calls to the Aboriginal Quitline following the campaign.
The Aboriginal and Torres Strait Islander Smoking Cessation Program in the ACT, supports a number of smoking cessation activities in the region, with an emphasis on pregnant smokers and their families.
In Tasmania additional funds were provided to increase anti-tobacco media campaigns between 2013 and 2016. At the same time, the NTC–More Targeted Approach was implemented including materials developed for Indigenous Australians.
The Victorian Government has established key strategic partnerships with non-Government organisations, such as Quit Victoria and the Victorian Aboriginal Community Controlled Health Organisation (VACCHO), which have employed coordinators to specifically address Indigenous tobacco control initiatives.
Understanding smoking prevalence at more localised levels, among pregnant women and those living in remote areas, as well as effective strategies to maintain smoking cessation, are important.