3.08 Cultural competency
Page content
Why is it important?
Improving the cultural competency of health care services can increase Aboriginal and Torres Strait Islander peoples’ access to health care, increase the effectiveness of care that is received, and improve the disparities in health outcomes (Freeman et al, 2014). ‘Cultural competency requires that organisations have a defined set of values and principles, and demonstrate behaviours, attitudes, policies and structures that enable them to work effectively cross-culturally’ (Dudgeon et al, 2010).
Cultural competency can be measured directly (self-reporting on patient experience) or indirectly (e.g. discharge against medical advice, employment of Aboriginal and Torres Strait Islander health workers). However, there is limited data available on the cultural competence of health services (Paradies et al, 2014) or on the effectiveness of interventions to address cultural competency in health care for Indigenous peoples (Truong et al, 2014; Clifford et al, 2015).
The Cultural Respect Framework for Aboriginal and Torres Strait Islander Health 2016–2026: a national approach to building a culturally respectful health system, has been developed to embed cultural respect principles into the Australian health system (AHMAC NATSIHSC, 2017). Cultural respect is achieved when the health system is accessible, responsive and a safe environment for Aboriginal and Torres Strait Islander people, where cultural values, strengths and differences are respected. The Framework outlines six domains that underpin culturally respectful health service delivery: whole of organisation approach and leadership; communication; workforce development and training; consumer participation and engagement; stakeholder partnerships and collaboration; and data, planning, research and evaluation.
Findings
Monitoring and measuring cultural respect in the health system nationally is difficult. In this performance measure we have drawn from a range of national data collections which provide various perspectives from Aboriginal and Torres Strait Islander peoples on their experiences of the Australian health system.
In the 2014–15 Social Survey, 35% of Indigenous Australians aged 15 years and over reported that they had been treated unfairly in the previous 12 months because they are Aboriginal and/or Torres Strait Islander. Around 14% of Indigenous Australians reported that they avoided situations due to past unfair treatment. Of those, 13% had avoided seeking health care because of previous unfair treatment. A study of 755 Aboriginal Victorian adults found 30% had experienced racism in health settings in the previous 12 months (Kelaher et al, 2014).
While most Indigenous Australians had positive interactions with doctors, in the 2014–15 Social Survey around 6%of Indigenous Australians aged 15 years and over disagreed or strongly disagreed with the statement ‘Your doctor can be trusted’.
When asked about their experiences with doctors in 2014–15, Indigenous Australians in non-remote areas reported that their GP, rarely or never: showed respect for what was said (15%), listened to them (20%) or spent enough time with them (21%). National data for all Australians from the Patient Experience Survey showed that their doctor only sometimes, rarely or never: showed respect for what was said (7%), listened to them (10%) or spent enough time with them (11%) (ABS, 2015c).
In 2012–13, 70% of Indigenous Australians aged 15 years and over in non-remote areas gave an overall rating of the health care they received in the last 12 months as excellent or very good (ABS, 2013c).
In 2012–13, 30% of Aboriginal and Torres Strait Islander peoples reported that they did not access health care when they needed to in the previous 12 months. Of those people, reasons for not accessing care included: disliked service/professional or felt embarrassed/afraid (22%); felt it would be inadequate (9%); did not trust service or provider (9%); and discrimination/not culturally appropriate/language problems (4%). These types of barriers were higher for those needing to seek care from counsellors (45%) and hospitals (27%) compared with doctors and dentists (23%). Noting that cost (43%) was the major barrier to accessing dental services, dislike of service/professional or feeling embarrassed/afraid was also identified by 19%, which has links to poor oral health outcomes.
In 2014–15, of the estimated 46,700 Indigenous Australians reporting they mainly speak an Indigenous language (11% of Indigenous Australians aged 15 years and over), 38% reported having difficulty understanding and/or being understood in places where only English is spoken (ABS, 2016e).
Between July 2013 and June 2015, there were 18,427 hospitalisations of Aboriginal and Torres Strait Islander people where they left hospital against medical advice or were discharged at their own risk. This represented around 3% of all hospitalisations for Aboriginal and Torres Strait Islander peoples compared with 0.5% for non-Indigenous Australians (age-standardised).
In 2011, there were around 8,500 Aboriginal and Torres Strait Islander people employed in health-related occupations. Nursing (2,189) was the largest group followed by nursing support and personal care workers (1,435), and Aboriginal and Torres Strait Islander Health Workers (1,256). Between 1996 and 2011 the rate of Indigenous Australians employed in the health workforce increased from 96 per 10,000 to 155 per 10,000 (see measure 3.12).
Aboriginal and Torres Strait Islander Health Workers play an important role in improving cultural competency in health care delivery (Thompson, S et al, 2011). A small study in the cardiology unit of a WA hospital (Taylor, KP et al, 2009) found these health workers improved the cultural security of the care provided, reduced the number of discharges against medical advice and increased participation in cardiac rehabilitation. Participation rates in cardiac rehabilitation have been lower for Indigenous Australians although it has been shown to be effective in reducing coronary death by up to 25% (NHF & AHHA, 2010).
As at May 2015, Aboriginal Health Workers and Aboriginal Health Practitioners represented 14% of all full-time equivalent (FTE) positions within Indigenous primary health care services. Around half (53% or 3,873) of the FTE paid positions in Commonwealth-funded Indigenous primary health care organisations were occupied by Indigenous Australians (AIHW, 2016o).
In 2014–15, of the 163 Indigenous primary health care organisations who had a governing committee or board, 74% had a governing committee or board of which all members were Aboriginal and/or Torres Strait Islander.
The majority (97%) of all Indigenous PHC organisations (see measure 3.05) employed local Aboriginal and Torres Strait Islander peoples, 93% had accessible and appropriate client/community feedback mechanisms, 93% had a formal organisational commitment to achieving culturally safe health care, 90% provided cultural orientation for non-Indigenous staff and 83% had mechanisms for gaining high-level advice on cultural matters affecting service delivery. Cultural group activities (e.g. art, hunting, bush outings) were provided by 47%of Indigenous primary health care organisations and 73% of Aboriginal and Torres Strait Islander organisations funded to provide substance-use services. Eighteen per cent of Indigenous primary health care organisations offered bush tucker nutrition programs and 11% offered bush medicine.
A private GP practice in Qld found that by working in partnership with the Indigenous community the number of Indigenous patients increased from 5 to 40 per month. Strategies introduced included bulk billing, one session per week specifically for Indigenous patients and a bus to the clinic. In addition, cultural safety training was undertaken by staff and an Indigenous health worker attended the clinic to assist with cultural safety and referrals (Johanson & Hill, 2011).
Figures
Figure 3.08-1
Aboriginal and Torres Strait Islander primary health care organisations, by proportion of services with cultural safety policies or processes in place, 2014–15
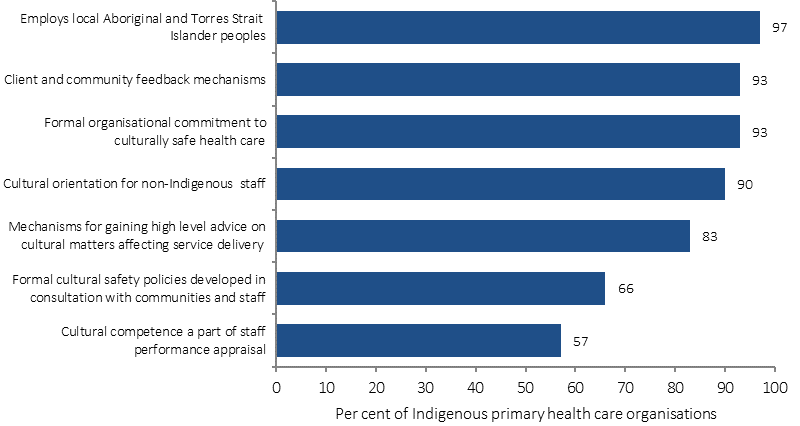
Source: AIHW analyses of 2014–15 OSR data collection
Figure 3.08-2
Aboriginal and Torres Strait Islander people employed in select health-related occupations, rates (per 10,000), 1996, 2001, 2006 and 2011
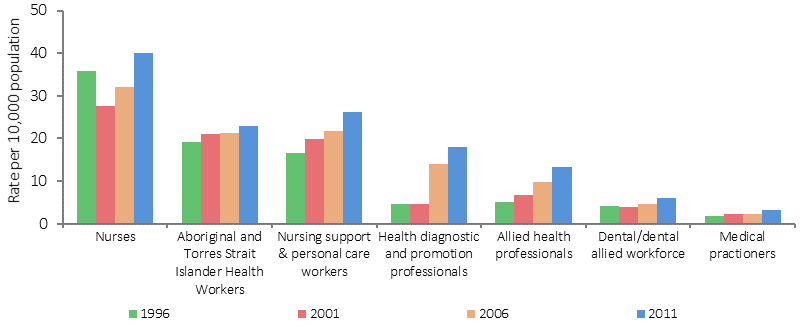
Source: AIHW analysis of ABS Census data
Figure 3.08-3
Reasons Indigenous Australians did not access health services when needed to, 2012–13
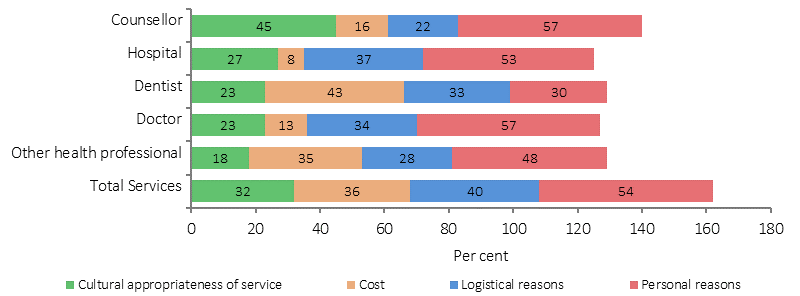
Note: more than one response allowed, sum may exceed 100%
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Table 3.08-1
Indigenous Australians who did not access health services when needed to, and reasons relating to cultural appropriateness,2012–13
| Dentist | Doctor | Other health professional | Hospital | Counsellor | Total health services | |
|---|---|---|---|---|---|---|
| Per cent | ||||||
| Did not access service when needed to in last 12 months | 21 | 14 | 9 | 6 | 6 | 30 |
| Reason(s) did not access service | ||||||
| Discrimination/ not culturally appropriate/ language problems | 2† | 3† | 2† | 4† | 4† | 4 |
| Dislikes service/professional, embarrassed, afraid | 19 | 14 | 13 | 14 | 27 | 22 |
| Felt it would be inadequate | 1† | 9 | 5 | 9 | 18 | 9 |
| Does not trust service provider | 4 | 6 | 3 | 8 | 12 | 9 |
| Cultural appropriateness of service (subtotal) | 23 | 23 | 18 | 27 | 45 | 32 |
† Estimate has a relative standard error between 25% and 50% and should be used with caution.
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Figure 3.08-4
Patient experience, Indigenous Australians aged 15 years and over who saw a doctor or specialist, non-remote areas, 2014–15
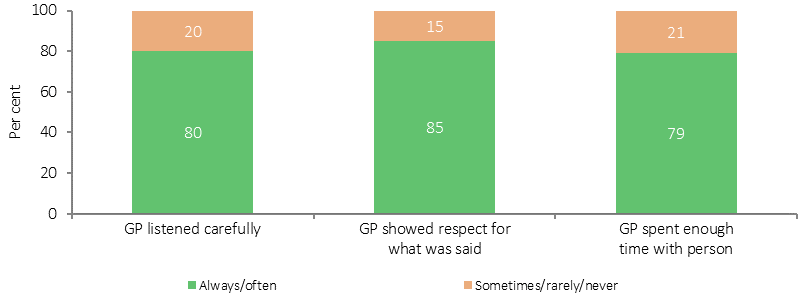
Source: ABS and AIHW analysis of 2014–15 NATSISS
Implications
There are key gaps in the evidence on the cultural competency of health services in Australia.
To Aboriginal and Torres Strait Islander peoples the term ‘health’ means not just the physical wellbeing of an individual but refers to the social, emotional and cultural wellbeing of the whole community in which each individual is able to achieve their full potential as a human being thereby bringing about the total wellbeing of their community. Australian governments have focused on improving the cultural competency of health services in several ways.
The National Aboriginal and Torres Strait Islander Health Plan 2013–2023 (NATSIHP) draws attention to ‘the centrality of culture in the health of Aboriginal and Torres Strait Islander peoples and the rights of individuals to a safe, healthy and empowered life’. Achieving improvements in health outcomes for Indigenous Australians means working towards fulfilling the vision of the NATSIHP; a health system that is free of racism and inequality and where all Aboriginal and Torres Strait Islander people have access to health services that are effective, high quality, appropriate and affordable.
In 2015, the Australian Government released the Implementation Plan for the NATSIHP, which includes activities intended to deliver against the following strategy: Mainstream health services are supported to provide clinically competent, culturally safe, accessible, accountable and responsive services to Aboriginal and Torres Strait Islander peoples in a health system that is free of racism and inequality.
The development and delivery of well-designed and implemented cultural safety training programs can assist in the aim of achieving a health system that is a safe environment for Aboriginal and Torres Strait Islander peoples and where cultural differences are respected. The Department of Health funded the development of the Aboriginal and Torres Strait Islander Health Curriculum Framework. The framework supports higher education providers to implement Aboriginal and Torres Strait Islander health curricula across their health professional training programs. Developed with extensive input and guidance from a wide range of stakeholders around Australia, the framework aims to prepare graduates across health professions to provide culturally safe health services to Aboriginal and Torres Strait Islander peoples through the development of cultural capabilities during their undergraduate training.
Aboriginal and Torres Strait Islander health professional organisations are funded to support and increase the capacity of the Aboriginal and Torres Strait Islander health workforce and contribute to promoting a culturally appropriate health care system with improved access to services and improved health outcomes for Aboriginal and Torres Strait Islander peoples. They contribute to increasing the number of health care providers delivering culturally appropriate care by providing advice, cultural safety training and practical support for employers, as well as providing advice to Government and other stakeholders on issues affecting the Aboriginal and Torres Strait Islander health workforce.
Australian Government funding is also provided to the Leaders in Indigenous Medical Education Network, which focuses on improving the quality and effectiveness of teaching and learning of Indigenous health in medical education through a nationally agreed curriculum framework, and for promoting best practice in the recruitment and retention of Indigenous medical students.
A key document to guide national Aboriginal and Torres Strait Islander health workforce policy and planning in relation to providing culturally safe and responsive health care is the National Aboriginal and Torres Strait Islander Health Workforce Strategic Framework (2016–2023), which has been developed within the overall policy context of the NATSIHP.
The Practice Incentives Program—Indigenous Health Incentive (PIP–IHI) supports general practices and Indigenous health services to provide better health care for Aboriginal and Torres Strait Islander patients. Payments are made to practices that register for the PIP–IHI and meet certain requirements, one of which is having at least two staff members from the practice (one of whom must be a GP) completing appropriate cultural awareness training. In 2014–15, about 3,700 general practices and Indigenous health services had signed on to the incentive and around 64,700 patients were registered.
The Australian Commission of Safety in Health Care is developing a guide on strategies and best practice for mainstream services (including acute care) in the delivery of care for Indigenous Australians.
The Australasian College for Emergency Medicine has developed a series of educational tools and resources designed for doctors to enhance culturally competent communication and overall care for Aboriginal and Torres Strait Islander patients in the emergency department.
The Aboriginal and Torres Strait Islander Healing Foundation found that understanding and addressing trauma can have a positive effect on people’s lives, relationships and workplaces. Since 2012, the Foundation has supported 62 community education and workforce development projects around Australia. One of the key aims of the projects is to build a workforce with increased capacity to recognise and respond to trauma, loss and grief. The current funding agreement (2015–18) allocates $3.6 million for trauma-informed Indigenous healing education and workforce development; and capacity building and knowledge creation for service providers of healing programmes. In 2014–15, 84.5% of all participants in trauma education projects reported that they can now better manage the impact of trauma. A further $14 million has been allocated for other healing programmes.
A WA report on cancer care (Thompson, S et al, 2011) made several practical recommendations to improve the cultural competency of care for Aboriginal patients including: providing a welcoming environment through welcome to country services, yarning places and access to traditional foods; facilitating the return of Aboriginal patients to their homelands for continued care where possible; ensuring that there is access to Aboriginal interpreters for Aboriginal people who are not confident speakers of English, and that staff understand differences in Aboriginal verbal and non-verbal communication styles; and ensuring service providers are familiar with, acknowledge and respect Aboriginal family structures, culture and life circumstances.
An evaluation of the Victorian government’s Koolin Balit investment is showing improvements in cultural responsiveness and cultural safety for Aboriginal people in some Victorian hospitals.
The ACT Health Aboriginal and Torres Strait Islander Health Impact Statement is a tool to assess the needs of Aboriginal and Torres Strait Islander peoples in relation to policies as they are in development.