1.24 Avoidable and preventable deaths
Page content
Why is it important?
Avoidable and preventable mortality refers to deaths from conditions that are considered avoidable given timely and effective health care (including disease prevention and population health initiatives) (Page et al, 2007; AIHW, 2010b). Avoidable deaths have been used in various studies to measure the quality, effectiveness and/or accessibility of the health system. Deaths from most conditions are influenced by a range of factors in addition to health system performance, including the underlying prevalence of conditions in the community, environmental and social factors and health behaviours.
Findings
In the period 2011–15, there were 6,427 deaths of Aboriginal and Torres Strait Islander people aged 0–74 years from avoidable causes in NSW, Qld, WA, SA and the NT combined. This represented 61% of all deaths of Aboriginal and Torres Strait Islander peoples aged 0–74 years. In contrast, deaths from avoidable causes for non-Indigenous Australians represented 50% of all non-Indigenous deaths in this age group.
After adjusting for the difference in age structure between the two populations, Aboriginal and Torres Strait Islander peoples died from avoidable causes at 3.3 times the rate of non-Indigenous Australians. The avoidable mortality rate of Aboriginal and Torres Strait Islander peoples was higher than that of non-Indigenous Australians in all age groups, and particularly high (4 times that of non-Indigenous Australians) in the middle adult age groups (35–54 years). Indigenous avoidable mortality rates were lowest in NSW (244 per 100,000) and highest in the NT (629 per 100,000).
There was a 32% decline in the avoidable mortality rate for Aboriginal and Torres Strait Islander peoples in the period 1998 to 2015. A study in the NT found a rapid fall in avoidable mortality between 1985 and 2004 in the Indigenous population for conditions amenable to medical care. This suggests that improvements in health care have made a major contribution to the fall in death rates and is consistent with observed improvements in perinatal survival, congenital malformations, stroke and hypertensive conditions, pneumonia and asthma, and infectious diseases (Li, SQ et al, 2009).
Among Aboriginal and Torres Strait Islander peoples, the most common conditions or events causing avoidable mortality were ischaemic heart disease (22%), diabetes (12%), suicide (11%), chronic obstructive pulmonary disease (COPD) (7%), road traffic injuries (7%) and cancer (7%). After adjusting for the difference in age structure, the conditions contributing the most to the avoidable mortality gap between Indigenous and non-Indigenous Australians were ischaemic heart disease (26% of the gap), diabetes (19% of the gap) and COPD (11% of the gap).
Figures
Figure 1.24-1
Age-standardised mortality rates for avoidable causes of death, Indigenous and non-Indigenous Australians aged 0–74 years, 1998 to 2015
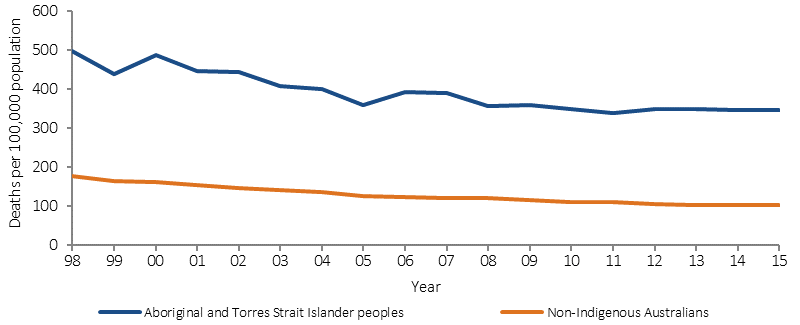
Source: ABS and AIHW analysis of National Mortality Database
Figure 1.24-2
Age-standardised mortality rates for avoidable causes of death by Indigenous status, NSW, Qld, WA, SA and NT, persons aged 0–74 years, 2011–15
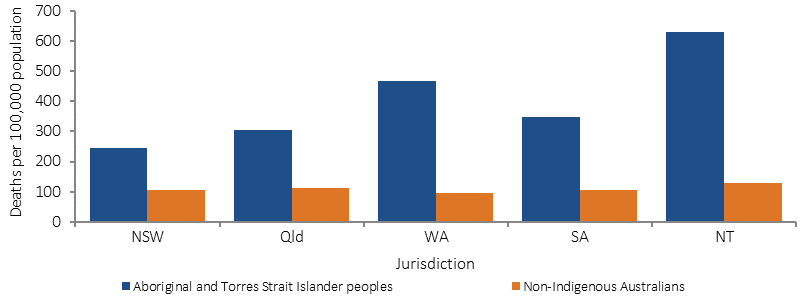
Source: ABS and AIHW analysis of National Mortality Database
Table 1.24-1
Avoidable mortality, by cause of death and Indigenous status, persons aged 0–74 years, NSW, Qld, WA, SA, and the NT, 2011–15(a)
Cause of death |
Per cent | Age-standardised rate per 100,000 | Rate ratio | Rate difference | Rate difference per cent | ||
|---|---|---|---|---|---|---|---|
| Indigenous | Non-Indigenous | Indigenous | Non-Indigenous | ||||
| Ischaemic heart disease | 21.8 | 19.6 | 83.1 | 19.9 | 4.2 | 63.2 | 26.4 |
| Diabetes | 12.0 | 4.6 | 50.6 | 4.7 | 10.8 | 45.9 | 19.2 |
| Suicide | 10.7 | 9.6 | 24.0 | 11.2 | 2.1 | 12.8 | 5.3 |
| Chronic obstructive pulmonary disease (COPD) | 7.3 | 7.4 | 34.8 | 7.4 | 4.7 | 27.5 | 11.5 |
| Cancer | 6.9 | 25.4 | 27.9 | 25.9 | 1.1 | 2.0 | 0.8 |
| Cervical cancer | 0.9 | 0.7 | 3.1 | 0.7 | 4.3 | 2.3 | 1.0 |
| Transport accidents | 6.6 | 4.9 | 15.7 | 5.6 | 2.8 | 10.1 | 4.2 |
| Cerebrovascular diseases | 4.8 | 6.7 | 20.2 | 6.9 | 2.9 | 13.3 | 5.6 |
| Complications of the perinatal period | 4.1 | 2.1 | 5.0 | 2.5 | 2.0 | 2.5 | 1.1 |
| Selected invasive infections | 4.1 | 3.0 | 14.2 | 3.1 | 4.5 | 11.0 | 4.6 |
| Assault | 3.1 | 0.8 | 7.3 | 1.0 | 7.5 | 6.3 | 2.6 |
| Renal failure | 2.5 | 1.3 | 10.9 | 1.3 | 8.6 | 9.7 | 4.0 |
| Rheumatic and other valvular heart disease | 2.1 | 1.3 | 7.6 | 1.3 | 5.7 | 6.2 | 2.6 |
| Other | 13.9 | 13.3 | 43.9 | 14.7 | 3.0 | 29.2 | 12.2 |
| Total | 100.0 | 100.0 | 345.2 | 105.4 | 3.3 | 239.8 | 100.0 |
| Total avoidable deaths 0–74 years | 6,427 | 87,332 | |||||
| Total deaths people 0–74 years | 10,589 | 175,217 | |||||
| Total deaths | 13,106 | 519,844 | |||||
(a) The avoidable mortality classification includes Acute lymphoid leukaemia/Acute lymphoblastic leukaemia (C91.0) for those aged 0–44 years only. This cause has been included in only the relevant age groups and the subset included in the total.
Source: ABS and AIHW analysis of National Mortality Database
Implications
Death rates for avoidable mortality among Aboriginal and Torres Strait Islander peoples are declining and the gap is closing. Chronic disease and injury are causing the greatest proportion of avoidable deaths for Aboriginal and Torres Strait Islander peoples and are amenable to both prevention and treatment. A study in the NT found that this decline has been greatest for conditions amenable to medical care, for example neonatal and paediatric care, antibiotics, immunisation, drug therapies, and improved intensive care and surgical procedures. Only marginal change was found for conditions responsive to public health (Li, SQ et al, 2009).
The Indigenous Australians’ Health Programme (IAHP) commenced from 1 July 2014, consolidating four existing funding streams (primary health care base funding, child and maternal health programmes, Stronger Futures in the Northern Territory and the Aboriginal and Torres Strait Islander Chronic Disease Fund), to improve the focus on local health needs, deliver the most effective outcomes, and better support efforts to achieve health equality between Aboriginal and Torres Strait Islander peoples and non-Indigenous Australians (see Policies and Strategies section).
The IAHP focuses on the prevention, early detection and management of chronic disease, including circulatory disease and diabetes through expanded access to and coordination of comprehensive primary health care. Activities funded under the IAHP include Tackling Indigenous Smoking; a care coordination and outreach workforce based in Primary Health Networks (PHNs) and Aboriginal Medical Services; and GP, specialist and allied health outreach services that support urban, rural and remote communities.
Diabetes is more common among Indigenous Australians than other Australians. Hospitalisations and death rates are both high, pointing to possible issues in secondary prevention. The Australian National Diabetes Strategy 2016–2020 seeks to prioritise Australia’s response to diabetes and its complications and comorbidities. Goal 5 is to reduce the impact of diabetes among Indigenous Australians.
Funding for Indigenous specific suicide prevention activity is an ongoing component of Commonwealth suicide prevention investment, as part of the new direction in suicide prevention outlined in the Government’s response to the National Mental Health Commission Review of Mental Health Programmes and Services. Approximately $5.6 million per annum is allocated to PHNs for the delivery of culturally appropriate suicide prevention services for Indigenous Australians, with approximately $0.7 million per annum to be allocated for a National Centre of Best Practice in Aboriginal and Torres Strait Islander Suicide Prevention.
Alive and Kicking Goals is a multi-award winning youth suicide prevention project based in the Kimberley region. The project aims to reduce the high suicide rate among Aboriginal and Torres Strait Islander youth through peer education workshops, one-on-one mentoring, and counselling. The project is wholly owned and led by young Aboriginal women and men.