3.11 Access to alcohol and drug services
Page content
Why is it important?
The 2014–15 Social Survey found that 31% of Indigenous Australians aged 15 years and over reported exceeding the alcohol guidelines for single occasion drinking and 31% reported using substances in the previous 12 months (see measures 2.16 and 2.17). The range of harms from alcohol and substance misuse includes chronic disease (e.g. liver disease), blood borne virus spread, injuries from motor vehicle accidents and assaults, incarceration, and social disruptions including family breakdown. Mental health issues are a common comorbidity and, along with poly-drug use, means that people presenting to alcohol and drug services typically have complex, multiple needs (NIDAC, 2014).
Alcohol and substance-use services provide a variety of interventions and support that seek to address harmful alcohol and other drug use, and restore the physical, social and emotional wellbeing of clients and their families (NIDAC, 2014). Services are delivered in residential and non-residential settings, in stand-alone facilities or as part of primary care services.
Access to these services by Indigenous Australians may be impacted by geography (e.g. distance to services, transport availability and road quality); the cultural competency of services (see measure 3.08); affordability (e.g. service, pharmaceutical and travel costs); and the availability of health professionals. Additional barriers include cultural beliefs and attitudes, such as shame associated with seeking treatment, concern about getting into trouble with the law and fear of losing their children (NIDAC, 2014).
Findings
The 2014–15 Online Services Report (OSR) included data from 67 Commonwealth-funded organisations that provided substance-use services for Indigenous Australians. These organisations provided 151,000 episodes of care to 25,196 clients, 84% of whom were Indigenous Australians. The distribution of clients in inner regional areas was 2% compared with 38% in major cities, 25% in remote, 22% in very remote and 13% in outer regional areas (AIHW, 2016o).
For Indigenous clients, these services provided around 2,400 residential episodes of care, 13,900 sobering-up, residential respite episodes of care, and 116,200 non-residential, follow-up and aftercare episodes of care.
Most organisations reported alcohol as one of their five most common substance use issues (96%), followed by cannabis (88%), amphetamines (70%), multiple drug use (64%) and tobacco (57%). For amphetamine use, this was an increase from 45% in 2013–14.
Treatment types used by nearly all organisations included information and education (97%), support and case management (96%) and counselling (88%). Organisations provided a wide range of drug and alcohol programmes and activities, with the most common being community education (82%), group counselling (79%), crisis intervention (75%), cultural groups (73%) and support groups (64%). For most organisations, depression (78%), anxiety/stress (73%) and grief/loss (72%) were key social and emotional wellbeing issues reported in terms of staff time and organisational resources, highlighting the known inter-relationship between substance use and mental health.
The 2014–15 Alcohol and Other Drug Treatment Services National Minimum Data Set included data from around 850 publicly funded drug and alcohol services (including some which also reported to the OSR). These services provided around 25,100 episodes of care to 17,400 Indigenous clients (representing 16% of total episodes and 15% of total clients). The Indigenous rate (3,140 clients per 100,000) was 7 times the non-Indigenous rate (457 clients per 100,000).
Indigenous clients tended to be younger than non-Indigenous clients, with the proportion of episodes in the 10–19 and 20–29 year age groups higher for Indigenous clients. The average distance travelled for treatment was greater for Indigenous clients (123km) than for non-Indigenous clients (53km) (AIHW, 2016i).
Alcohol was the principal drug of concern for 46% of Indigenous clients compared with 36% for non-Indigenous clients. The Indigenous rate for alcohol use was 9 times the non-Indigenous rate. For both Indigenous and non-Indigenous clients, the main drugs treated following alcohol were cannabis, amphetamines and then heroin (with Indigenous rates 5–7 times the non-Indigenous rates).
The main treatment types involved in episodes for Indigenous clients were counselling (42%), assessment only (18%), information and education only (10%), support and case management only (9%), rehabilitation (8%), withdrawal management (8%) and pharmacotherapy (2%) (AIHW, 2016i).
The majority of the 203 Commonwealth-funded Indigenous primary health care organisations provided care in relation to drug and alcohol issues. Alcohol, tobacco, cannabis, amphetamines and multiple drug use were the most common conditions managed in terms of staff time and organisational resources.
Based on GP survey data (2010–15), the rate at which GPs managed mental health related problems for drug abuse and alcohol misuse at encounters with Indigenous Australians was 2 and 3 times the rate respectively of other patients (after adjusting for differences in the age profile of the two populations). In the same period, GPs offered Indigenous patients counselling or advice on alcohol at 2 times the rate for other patients. Alcohol counselling or advice represented 1.3% of all clinical and therapeutic treatments provided to Indigenous Australians (compared with 0.7% of advice to other Australians).
During the period July 2013 to June 2015, there were approximately 9,800 hospitalisations related to alcohol use for Indigenous Australians and 8,500 due to drug use. After adjusting for difference in the age structure of the two populations, Indigenous males were 4 times as likely to be hospitalised for alcohol use as non-Indigenous males and Indigenous females were 3.6 times as likely as non-Indigenous females. Indigenous Australians were also 2.7 times as likely to be hospitalised for diagnoses related to drug use as non-Indigenous Australians.
In 2015, on a ‘snapshot day’, over 3,200 Indigenous clients received pharmacotherapy treatment for opioid dependence (NSW, Qld, SA, Tas, ACT and the NT combined), accounting for 10% of all clients. Indigenous clients were around 3 times as likely to have received pharmacotherapy treatment as non-Indigenous clients and tended to be younger, with higher proportions of clients in the age groups between 15 and 39 years (AIHW, 2016h). While 60% of Indigenous prison entrants had used illicit drugs in the previous 12 months and 54% reported a high risk of alcohol-related harm in the previous 12 months in 2015, 2% of Indigenous prisoners in custody received medication for opioid dependence and 9% accessed an alcohol treatment program while in prison (AIHW, 2015d).
Figures
Table 3.11-1
Episodes of care provided to Indigenous clients of Commonwealth-funded Indigenous substance-use services, 2014–15
| Episode type | Number |
|---|---|
| Residential treatment/ rehabilitation episodes of care | 2,400 |
| Sobering-up/residential respite episodes of care | 13,900 |
| Non-residential/follow-up/ aftercare episodes of care | 116,200 |
Source: AIHW 2016
Figure 3.11-1
Common substance use issues reported by Commonwealth-funded Indigenous substance-use services, 2014–15
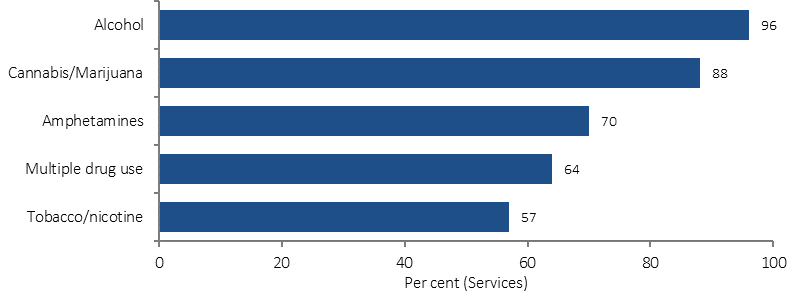
Source: AIHW 2016
Figure 3.11-2
Alcohol and other drug services treatment episodes by Indigenous status and age group, 2014–15
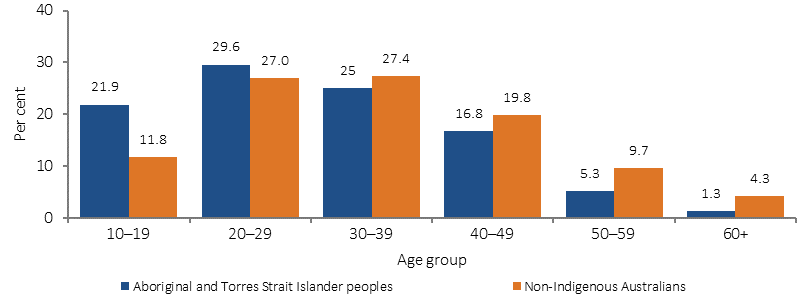
Source: AODTS NMDS (AIHW 2016)
Figure 3.11-3
Age-standardised hospitalisations with principal diagnoses related to alcohol use and drug use, by Indigenous status and sex, July 2013–June 2015
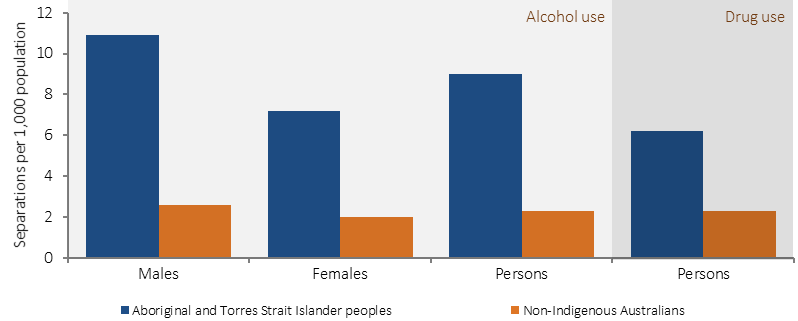
Source: AIHW analysis of National Hospital Morbidity Database
Implications
Due to the complex, often chronic and relapsing nature of drug and alcohol conditions, a greater intensity of treatment services are required and these need to have a long-term focus, be broader than clinical responses and include the provision of social support services (Gray, D et al, 2014). Mental health and social and emotional wellbeing issues are common comorbidities.
Key themes identified for effective alcohol treatment for Indigenous Australians included: individual engagement, flexibility, assessment of suitability, Aboriginal staff, community engagement, practical support, counselling, coping with relapse, and contingency planning (Brett et al, 2014). A recent literature review found no evidence on effective methamphetamine treatments for Indigenous Australians (MacLean et al, 2015).
The National Drug Strategy 2010–2015 (NDS) (currently being updated) provides the framework for an integrated and coordinated approach across all levels of government to reduce drug-related harm and use in Australia. Under the NDS, the National Aboriginal and Torres Strait Islander Peoples Drug Strategy 2014–19 aims to improve health and wellbeing by preventing and reducing the harmful effects of alcohol and drugs on individuals, families, and communities.
The Indigenous Advancement Strategy–Safety and Wellbeing Programme provides funding for strategies to enhance wellbeing and community safety. This includes funding support for a range of alcohol and other drug treatment services across Australia. In 2015–16, funding was provided to over 80 alcohol and other drug service providers to improve access to culturally appropriate treatment, prevention, rehabilitation, education and aftercare services for Indigenous Australians, particularly in rural and remote areas.
In 2015–16, 25 Aboriginal and Torres Strait Islander service providers were funded through the Commonwealth Substance Misuse Service Delivery Grants Fund and Non-Government Organisation Treatment Grants Programme to deliver a range of alcohol and other drug treatment and rehabilitation services. In addition, the majority of Indigenous Primary health care organisations funded through the Indigenous Australians’ Health Programme provided care in relation to alcohol and drugs.
As part of the December 2015 response to the National Ice Taskforce’s Final Report, $241.5 million was allocated to Primary Health Networks (PHNs) to commission additional drug and alcohol treatment services with $78.6 million allocated specifically for treatment services for Indigenous Australians. PHNs are to pursue holistic approaches to Indigenous drug and alcohol treatment that are culturally safe, competent and respectful in both Indigenous specific and mainstream services.
In recognition of the acute need in the NT, the Commonwealth supports additional effort such as dry community declarations (Alcohol Protected Areas) and the power to amend liquor licenses and permits. The Commonwealth is also providing around $91.5 million over 7 years (to 2022) to tackle the harms caused by alcohol under the new National Partnership on Northern Territory Remote Aboriginal Investment.
The Strong Spirits, Strong Minds media campaign, developed from a strong cultural foundation with input from an Aboriginal youth advisory panel, aims to prevent and/or delay the early uptake of alcohol and other drugs by young Aboriginal people in Perth. The Ngunnawal Bush Healing Farm will provide a culturally appropriate alcohol and other drug residential rehabilitation facility for adult Aboriginal and Torres Strait Islander people in the ACT.