3.19 Accreditation
Page content
Why is it important?
Accreditation is a process, usually voluntary, through which a recognised external body assesses the extent to which a health care organisation meets applicable quality standards. Quality standards typically address issues such as governance of the organisation, management of safety issues such as infection control, handling of care processes such as discharge planning, general management issues such as human resource management, quality of the physical infrastructure, and issues such as handling of patient complaints. Assessments of quality often result in recommendations for action. The assessment outcome may also be reported publicly in a summarised form.
The services accessed by Aboriginal and Torres Strait Islander peoples should be able to demonstrate a comparable level of quality when compared with other health services in Australia. While accreditation status is a broad measure, it provides one measure of the capability of services, based on their skills and knowledge, to provide quality health services to Aboriginal and Torres Strait Islander peoples.
In Australia, there are accreditation systems for both hospitals and general practice. Public and private hospitals are accredited against the National Safety and Quality Health Service Standards (NSQHSS). There are nine organisations approved by the Australian Commission on Safety and Quality in Health Care (ACSQHC) to asses to the NSQHSS. There are currently 1,342 public and private hospitals and day procedure services in Australia eligible to be assessed against the NSQHSS. Of these health service organisations, 743 (55%) are in the public sector and 599 (45%) are in the private sector.
In 2014–15, 93% of public hospitals, were accredited (AIHW, 2016b). For small hospitals located in regional and remote areas, accreditation is less common. Achieving accreditation generally requires a considerable ongoing investment of time and resources, which is not always easy for smaller hospitals. It is not possible to draw conclusions about the quality of care in hospitals that do not have accreditation.
Accreditation in general practice involves assessment against standards set by the Royal Australian College of General Practitioners (RACGP) in five key areas: practice services; rights and needs of patients; safety, quality improvement and education; practice management; and physical factors (RACGP, 2010). There are two registered accreditation providers: Australian General Practice Accreditation Limited (AGPAL) and General Practice Accreditation Plus (GPA+). In addition to patient safety and service quality, there is evidence that the process of accreditation encourages quality improvement and continuing professional development (URBIS, 2014). It is likely that more practices are using the standards than are actually accredited at any one time (SCRGSP, 2016a).
The Practice Incentives Program (PIP) has helped increase rates of general practice accreditation (ANAO, 2010). Note, though that Aboriginal Medical Services and other practices in remote locations or with specialist interests are often not eligible for accreditation against RACGP Standards or find the process of accreditation difficult.
Findings
Between July 2014 and June 2015, 92% of public hospital separations for Aboriginal and Torres Strait Islander peoples occurred in accredited hospitals (as did 93% of public hospital separations for non-Indigenous Australians). Rates were lowest in outer regional areas, and highest in remote areas.
In most jurisdictions over 90% of public hospital separations for Indigenous Australians occurred in accredited hospitals. The exceptions were Qld (74%) and Tas (59%). In Qld the proportion of accredited separations was over 10 percentage points lower for Indigenous patients than for non-Indigenous patients; however in WA the Indigenous proportion was over 10 percentage points higher. In the other jurisdictions Indigenous and non-Indigenous proportions were similar.
In 2014–15, 92% of general practices registered with GPA+ or AGPAL were fully accredited by the respective organisation. The proportion of practices that were accredited ranged from 92% for practices in areas where Aboriginal and Torres Strait Islander peoples make up less than 2% of the population, to 95% in areas where 10% or more of the population is Indigenous.
The 2014–15 Online Services Report (OSR) includes data on the accreditation status of Commonwealth-funded Indigenous primary health care organisations.
Of the 203 organisations, 157 employed a GP and of those, 91% reported having a current clinical RACGP and/or organisational accreditation. The 203 organisations included 138 Commonwealth-funded Aboriginal and Community Controlled Health Organisations, of which 129 employed a GP. 98% of those 129 organisations reported RACGP and/or organisational accreditation.
Figures
Figure 3.19-1
Proportion of public hospital separations in accredited hospitals, by Indigenous status and state/territory, 2014–15
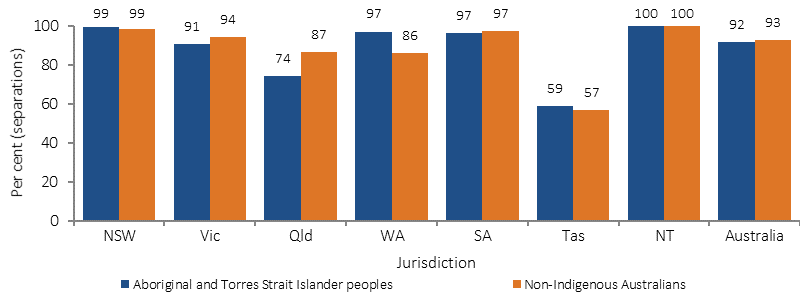
Note: Data are from public hospitals only. Data for the ACT individually were not available.
Source: AIHW analysis of National Hospital Morbidity Database, National Public Hospitals Establishment Database and ACSQHC unpublished data
Figure 3.19-2
Proportion of public hospital separations in accredited hospitals, by Indigenous status and remoteness, Australia, 2014–15
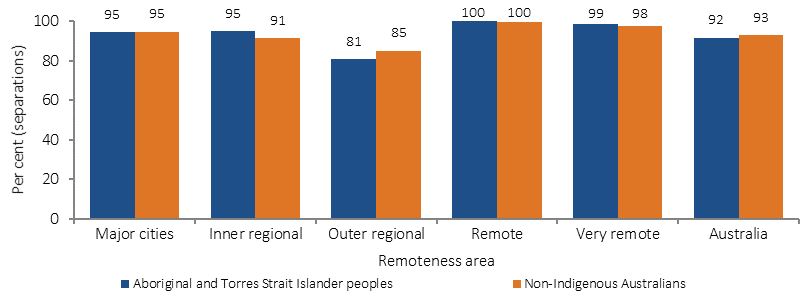
Note: Data are from public hospitals only.
Source: AIHW analysis of National Hospital Morbidity Database, National Public Hospitals Establishment Database and ACSQHC unpublished data
Figure 3.19-3
Proportion of general practices accredited through AGPAL and GPA+, by proportion of the population that is Indigenous, 2014–15
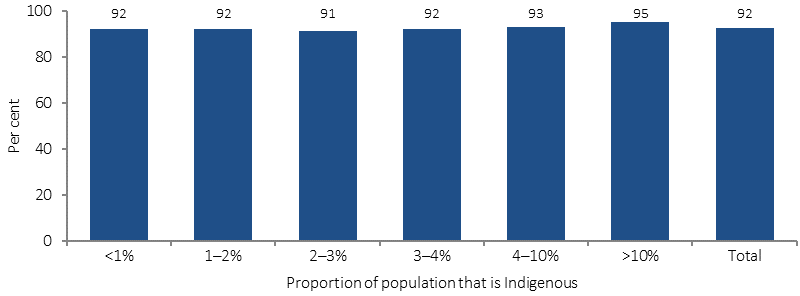
Source: AIHW analysis of AGPAL and GPA+ data
Implications
By achieving accreditation, health service organisations can monitor, evaluate and improve the quality of health services they provide.
In 2014–15 the Australian Government expanded the Healthy for Life (HfL) programme to build continuous quality improvement (CQI) into clinical practice and service delivery within Aboriginal Community Controlled Health Organisations (ACCHOs). Funding was also provided to the Aboriginal Community Controlled Health Sector peak bodies to support ACCHOs in implementing best practice clinical, governance and business systems and to provide training and support to ACCHOs in the use of CQI to achieve improved clinical outcomes.
The ACSQHC is undertaking a project to improve the care provided to Aboriginal and Torres Strait Islander people in health service organisations, using the framework of the NSQHSS. Now underway, the next stage of this project aims to:
- raise awareness of the issues facing Aboriginal and Torres Strait Islander patients in mainstream health service organisations
- improve the safety and quality of care for Aboriginal and Torres Strait Islander patients by supporting mainstream organisations to implement the NSQHSS, using resources that contain effective, evidence-based strategies to address Indigenous health issues
- improve the Aboriginal and Torres Strait Islander cultural awareness skills of the surveyor workforce whose members assess health service organisations to the NSQHSS.