1.15 Ear health
Page content
Why is it important?
Hearing loss among Aboriginal and Torres Strait Islander peoples is widespread and much more common than for non-Indigenous Australians (Burns & Thomson, 2013; Darwin Ottis Guidelines Group et al, 2010).
Otitis media is an inflammation of the middle ear. Otitis media with effusion involves a collection of fluid within the middle ear space. Chronic suppurative otitis media occurs with persistent discharge through a perforation in the eardrum and active bacterial infection within the middle ear space (Dawin Ottis Guidelines Group et al, 2010). Otitis media is a significant cause of hearing loss in Indigenous children and is characterised by earlier onset, higher frequency, greater severity and greater persistence than non-Indigenous children (Jervis-Bardy et al, 2014). Several studies have found that Indigenous children living in remote communities experience high rates of severe and persistent ear infections (Edwards, J & Moffat, 2014; Morris et al, 2007; Gunasekera et al, 2009; Kong & Coates, 2009). Hearing loss, especially in childhood, can lead to linguistic, social and learning difficulties and behavioural problems in school. Such difficulties may reduce educational achievements and have lifelong consequences for wellbeing, employment, income, social success, contact with the criminal justice system and future potential (Williams, DR & Mohammed, 2009).
Otitis media is associated with poverty, crowded housing conditions and nutritional deficiencies (Burns & Thomson, 2013). Second hand smoke is a cause of middle ear infection, including otitis media (Office on Smoking & Health (US), 2006).
Findings
Self-reported survey data may under-estimate health conditions as it only includes conditions diagnosed by a doctor or nurse. There has been a significant decline in the national proportion of Indigenous children aged 0–14 years with self-reported ear or hearing problems, from 11% in 2001 to 8% in 2014–15 (ABS, 2016e). In remote areas the decline was steeper, from 18% to 11%. However, in 2014–15 the proportion of Indigenous children with ear/hearing problems was still 2.9 times the rate for non-Indigenous children. The NT and WA had the highest rate for Indigenous children with hearing problems (11% and 10% respectively) and Tasmania/ACT the lowest (5%). Deafness was reported for 3.0% of Indigenous children, otitis media for 2.9% and other ear diseases 3.5%. In 2014–15, of those Indigenous children aged 0–14 years with ear and hearing problems, 83% received some form of treatment including medication (48%), check by an ear/hearing specialist (46%) and surgery (31%); while 16% did not have any treatment for their ear and hearing problems. Note for some forms of ear disease the protocol is to ‘watch and wait’ (Darwin Ottis Guidlines Group et al, 2010).
The 2012–13 Health Survey collected comprehensive long-term health condition data for all age groups. In 2012–13, 12% of all Indigenous Australians reported an ear or hearing problem. The pattern of ear health problems varies with age. Otitis media is more prevalent in children while reported deafness increases steadily with age. In 2012–13, deafness was reported for 3% of Indigenous children, with rates rising steadily to 26% of those aged 55 years and over. In 2012–13, an ear or hearing problem was higher for Indigenous Australians than for non-Indigenous Australians in all age groups from 0–54 years of age. After adjusting for differences in the age structure of the two populations, otitis media among Indigenous Australians was 2.4 times as high as the non-Indigenous rate, with rate ratios of 1.4 for deafness and 1.3 for ear health problems overall. Indigenous Australians aged 15 years and over in the lowest household incomes were more likely to report ear/hearing problems than those in the highest incomes. Relationships were also evident for education.
Data is collected for Indigenous children and young people prioritised to receive Australian Government funded hearing outreach services in the NT. In 2015–16, 2,253 outreach audiology services were provided to 1,981 NT Indigenous children and young people, who gave consent to share the information with the AIHW through this programme. Among them, 49% had hearing loss (compared with 52% in 2012-13) and 32% had a hearing impairment (compared with 37% in 2012-13) (AIHW, 2017c). In 2015–16, of the 2,010 children and young people who received an audiology or ENT outreach service, 66% were diagnosed with at least one type of ear condition. The most common condition was otitis media with effusion (23%) followed by eustachian tube dysfunction (16%) and foreign body (16%). Among the 2,197 children who received 3 or more audiology or ENT services between August 2007 and June 2016, the proportion diagnosed with at least 1 ear condition decreased from 78% at the first service to 49% at the last service.
During the two years to June 2015, there were around 5,300 hospitalisations for Indigenous Australians for ear disease. The Indigenous rate (3.1 per 1,000) was similar to the non-Indigenous rate (2.6 per 1,000). Rates for Indigenous children aged 0–4 years were lower than those for non-Indigenous children, while for those aged 5–14 years the Indigenous rate was twice as high. For Indigenous children aged 0–14 years, the rate was twice as high in remote and very remote areas (14 and 15 per 1,000) as in major cities (6 per 1,000). Since 2004–05, there has been a 47% increase in ear-related hospitalisations for Indigenous children aged 0–14 years (no change for non-Indigenous children) and no significant change for those aged 15 years and over (10% increase for non-Indigenous Australians) in NSW, Vic, Qld, WA, SA and the NT combined.
In 2014-15, the rate of myringotomy procedures (incision in the eardrum to relieve pressure caused by excessive fluid build-up) in hospital was 1.2 per 1,000 in the population for Indigenous Australians and 1.7 per 1,000 for other Australians (AIHW 2016). The elective surgery median wait time for myringotomy procedures was 55 days for Indigenous patients compared with 57 days for other Australian patients (public hospital waiting lists) (AIHW, 2016x). In 2015–16, the elective surgery wait time for myringoplasty (repair of middle ear perforation) was 82 days longer for Indigenous patients than other patients (SCRGSP2017). In the period from July 2013 to June 2015, Indigenous children aged 0–14 years were hospitalised for tympanoplasty procedures (a reconstructive surgical treatment for a perforated eardrum) at 4 times the rate of non-Indigenous children. One in ten children fitted with a hearing aid or cochlear implant in 2010 were Indigenous (AIHW & AIFS, 2014a).
For Indigenous children aged 0–14 years, otitis media was managed by GPs at a similar rate (67 per 1,000 encounters) to that for other Australian children (64 per 1,000). Rates were also similar for total ear problems in 2010–15 (105 compared with 98). In 2014–15, 24% of Australian Government-funded Indigenous primary health services provided access to ENT specialists on site and 78% off site. In 2008–15, data collected through the Qld Deadly Ears programme showed that of 0–4 year-old clients who received an audiology assessment (1,788 children), 24% had hearing loss in both ears and 11% in one; for clients aged 5–14 years (4,646 children), 30% had hearing loss in both ears and 21% in one ear.
Figures
Figure 1.15-1
Age-standardised hospitalisation rates for diseases of the ear and mastoid process, by age and Indigenous status, NSW, Vic, Qld, WA, SA and the NT, 2004–05 to 2014–15
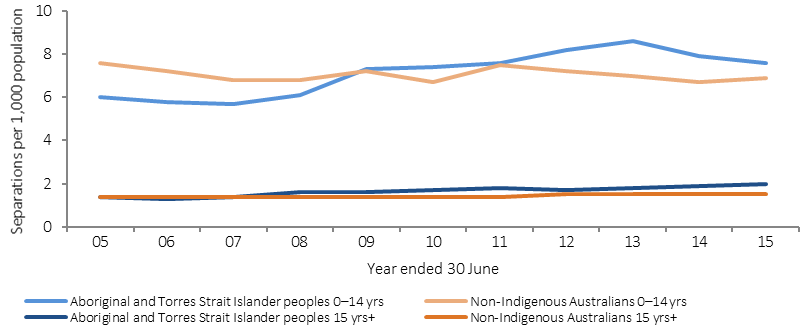
Source: AIHW analysis of National Hospital Morbidity Database
Figure 1.15-2
Ear and hearing problems managed by GPs, by Indigenous status of patients aged 0–14 years, April 2010–March 2011 to April 2014–March 2015
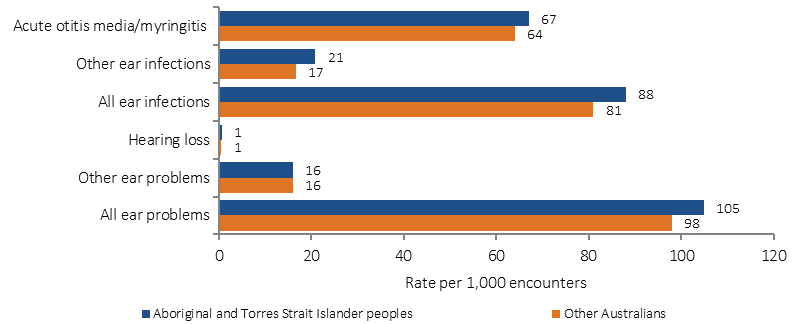
Source: Family Medicine Research Centre, University of Sydney analysis of BEACH data
Table 1.15-1
Long-term hearing problems children aged 0–14 years, by Indigenous status, by remoteness, 2001, 2004–05, 2008, 2012–13 and 2014–15
| Indigenous status | 2001 | 2004-05 | 2008 | 2012–13 | 2014-15 |
|---|---|---|---|---|---|
| Per cent | |||||
| Total Indigenous | 11 | 10 | 9 | 7 | 8 |
| Remote | 18 | 13 | 10 | 9 | 11 |
| Non-remote | 9 | 9 | 8 | 7 | 7 |
| Total non-Indigenous | 5 | 3 | 3 | 4 | 3 |
Source: ABS & AIHW analysis of 2001 NHS (Indigenous supplement), 2004–05 NATSIHS, 2008 NATSISS, 2012–13 AATSIHS and 2014–15 NATSISS
Implications
The current rate of GP management of ear or hearing problems for Indigenous children 0–14 years is 1.1 times the non-Indigenous rate yet the prevalence of ear disease is almost 3 times as high. The Indigenous hospitalisation rate for myringotomy is less for Indigenous Australians than non-Indigenous Australians (0.7 times) and there are longer wait times for myringoplasty procedures. Improving prevalence data beyond self-reported estimates is also a priority.
Evidence suggests that a comprehensive approach combining prevention, early treatment, and coordinated management is required. Primary prevention includes working with families on encouraging breastfeeding (Bowatte et al, 2015) eating a healthy diet, reducing exposure to second hand smoke, nasal passage clearing, seeking early medical assessment and encouraging vaccination. Once otitis media develops, medical management in line with the Recommendations for Clinical Care Guidelines on the Management of Otitis Media in Aboriginal and Torres Strait Islander populations is recommended. Screening for hearing loss and regular ear checks in the neonatal and pre-school period is recommended for Indigenous children given the high prevalence of otitis media. Once hearing loss is detected, access and referral to a range of health services is needed including speech therapists and audiology support services (Darwin Ottis Guidelines Group et al, 2010). If permanent hearing loss is detected, access and referral to support for hearing augmentation and other remedial therapies should be sought. Strategies in schools such as classroom management strategies, language therapy, and sound amplification have been successful tools for those with hearing impairment (Massie et al, 2004; Burrow et al, 2009; Burns & Thomson, 2013).
Around $36 million over the period 2013–14 to 2018–19 has been provided for ear health initiatives to assist in reducing the number of Indigenous Australians suffering avoidable hearing loss, and give Indigenous children a better start to education. Key initiatives include around $24 million over four years from 2013–14 for the Healthy Ears—Better Hearing, Better Listening Programme, which aims to increase access to clinical ear health services for Indigenous children and youth, with a focus on rural and remote areas. Services are provided by a range of professionals, including ENT specialists, audiologists and speech therapists. Funding is also available to streamline care pathways, train health professionals, supply equipment and diagnostic tools and continue to provide the Care for Kids’ Ears health promotion resources.
In 2015–16, $4.4 million was provided for the delivery of the Australian Hearing Specialist Program for Indigenous Australians through outreach sites including remote communities. A further $4.9 million was provided to Australian Hearing to deliver hearing services to eligible Indigenous Australians over 50 years of age.
State and territory governments have implemented a variety of programmes for Indigenous ear or hearing health. In Qld, the Deadly Ears Program works in 11 communities across rural and remote Queensland, delivering ear health services and building local capacity. In addition, the programme coordinates policy and practice changes across the health, early childhood and education sectors, provides training and development for health care professionals and educators, and undertakes research to improve prevention, treatment and management of middle ear disease and its impacts on early childhood development.
A number of Ear Health projects are delivered in the Kimberley region using an integrated, region-wide, planned and co-ordinated approach. A joint Ear Health Protocol has been developed with a strong focus on detection at an early age.