2.03 Environmental tobacco smoke
Page content
Why is it important?
Environmental tobacco smoke (also known as second hand smoke) is a significant cause of morbidity and mortality. The first evidence of harm to children from second hand smoke (Colley, 1974; Harlap & Davies, 1974; Leeder et al, 1976) and increased lung cancer risk in adults (Hirayama, 1981) emerged over 30 years ago. Global burden of disease analysis attributed 603,000 deaths to second hand smoke in 2004 (Öberg et al, 2011).
There is strong and consistent evidence that second hand smoke (SHS) causes lung cancer and ischaemic heart disease. It is also associated with increased risk of respiratory disease in adults, increases the risk of Sudden Infant Death Syndrome, and exacerbates asthma and ear infections such as otitis media in children (Thomas, DP & Stevens, 2014) (see measure 1.15). SHS is associated with increased risk of hospital readmission of Indigenous infants with bronchitis and hospital admission for Indigenous children for acute asthma (McCallum et al, 2016; Giarola et al, 2014). Exposure to SHS during pregnancy is also associated with an increased risk in neural tube defects (Wang, L et al, 2014).
The home is a key setting for exposure to SHS for pregnant women and young children. Exposure to parents’ smoking in childhood is found to have pervasive vascular health effects into adulthood (Gall et al, 2014). Overcrowding in housing (see measure 2.02) increases the risk of such exposure and developing asthma. Smoking in cars is also an important locus for child exposure to SHS (Agaku et al, 2014).
Smoke-free homes support successful smoking cessation (quit attempts and preventing relapse) along with a reduction in consumption of cigarettes (Thomas, DP & Stevens, 2014) (see measure 2.15). Qualitative research also suggests smoke-free homes are associated with reductions in young people taking up smoking (Thomas, DP & Stevens, 2014; Thomas, DP et al, 2015b).
Evaluation of a family-centred intervention to reduce infant exposure to SHS in Indigenous families concluded that all household members (not only the mother) should cease smoking from the time of conception (Walker et al, 2015).
Findings
In 2014–15, 59% of Indigenous people were living in households with daily smokers (ABS, 2016e). An estimated 138,000 Indigenous children aged 0–14 years were living in households with daily smokers, representing 57% of all Indigenous children in this age range, compared with 21% of non-Indigenous children. Furthermore, 13% of Aboriginal and Torres Strait Islander children lived in households with people who smoked at home indoors.
Between 2004–05 and 2014–15 there was a significant reduction in the proportion of Indigenous children aged 0–14 years living in households with daily smokers, falling from 68% to 57%. There was also a significant reduction for non-Indigenous children from 35% in 2004–05 to 21% in 2014–15.
In 2014–15, the proportion of Indigenous children aged 0–14 years living in households with daily smokers was 73% in remote areas (14% for non-Indigenous) compared with 53% in non-remote areas (21% for non-Indigenous). The proportion of Indigenous children aged 0–14 year living in households where smoking occurs indoors, ranged from 11% in major cities to 20% in very remote areas.
The proportion of Indigenous children aged 0–14 years living in households with daily smokers ranged from 51% in Victoria to 71% in the NT. The proportion of Indigenous children aged 0–14 years living in households where smoking occurs indoors, ranged from 7% in ACT to 17% in the NT .
Strong associations exist between the socio-economic circumstances of Indigenous households and whether children are exposed to SHS. The 2014–15 Social Survey results indicate that Indigenous children aged 0–14 years living in households with the lowest income quintiles were 6.6 times as likely to be exposed to tobacco smoke at home indoors compared with those living in the highest income households. There is a similar relationship with housing: 15% of children living in rental households had exposure to tobacco smoke where smoking occurred indoors compared with those living in homes that are owned or being purchased (7%).
Figures
Figure 2.03-1
Proportion of children aged 0–14 years living in households with daily smoker(s), by Indigenous status and state/territory 2014–15
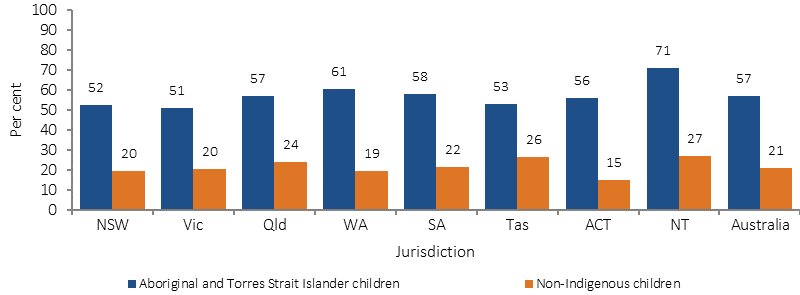
Source: ABS and AIHW analysis of 2014–15 NATSISS and 2014–15 NHS
Figure 2.03-2
Proportion of children aged 0–14 years living in households with daily smoker(s), by Indigenous status and remoteness, 2004–05, 2007–08, 2012–13 and 2014–15
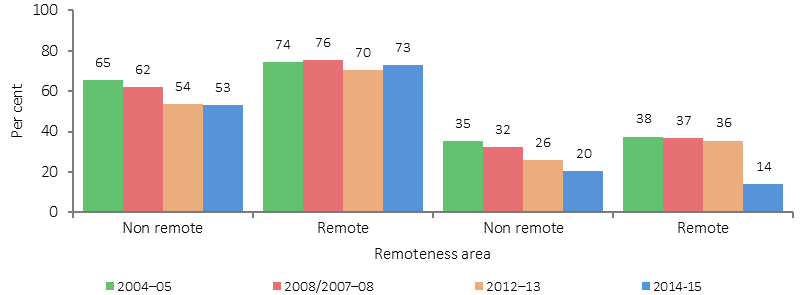
Source: ABS and AIHW analysis of 2004–05 NATSIHS, 2004–05 NHS, 2008 NATSISS, 2007–08 NHS, 2012–13 AATSIHS, 2014–15 NHS, 2014–15 NATSISS
Figure 2.03-3
Proportion of Indigenous children aged 0–14 years living in households where smoking occurs indoors, by remoteness, 2014–15
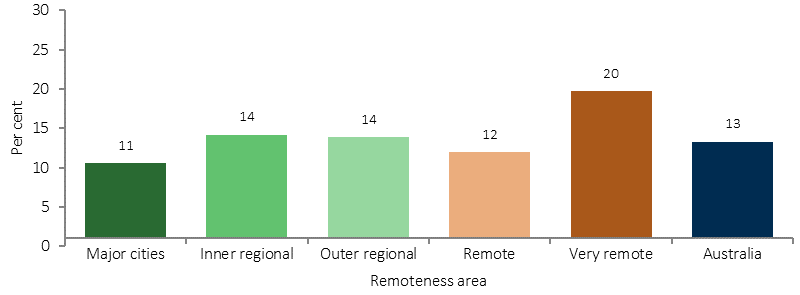
Source: ABS and AIHW analysis of 2014–15 NATSISS
Figure 2.03-4
Proportion of Indigenous Australians (all ages) living in households with daily smoker(s), by age, 2014–15
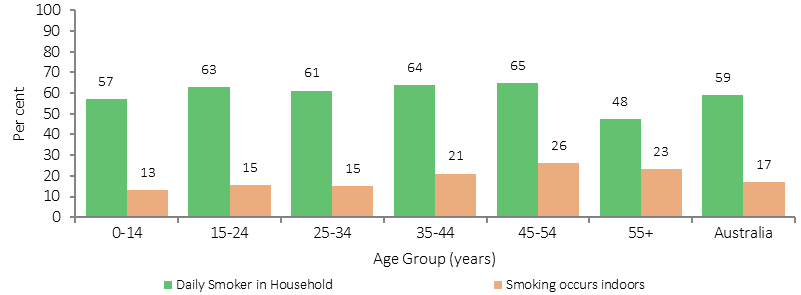
Source: ABS and AIHW analysis of 2014–15 NATSISS
Implications
The Australian Government has a range of policies and programmes in place that complement state and territory activity to reduce the harms from smoking. These policies and programmes include: excise increases on tobacco; education programmes and campaigns; plain packaging of tobacco products; labelling tobacco products with new, larger graphic health warnings; prohibiting tobacco advertising and promotion; and providing support for smokers to quit.
The National Tobacco Strategy 2012–2018 has nine priority areas for action, one being to reduce exceptions to smoke-free workplaces, public places and other settings.
Smoking is now banned in almost all indoor public places and increasingly in outdoor spaces, particularly where children are present. Most jurisdictions prohibit smoking in cars when children are present. The Northern Territory, Qld, Victoria, NSW and Tasmania have introduced complete smoking bans in their prisons.
The policy implications for addressing the dangers of second hand smoke are similar to those for tobacco smoking in general (see measure 2.15) and tobacco smoking during pregnancy (see measure 2.21), and should be monitored in conjunction with these measures.
In 2010, the Australian Government delivered a targeted Tackling Indigenous Smoking (TIS) programme to reduce Indigenous smoking rates. Following the review of the programme in 2014, the revised TIS program now funds regional projects to deliver a range of evidence-based activities that suit the local context and the needs of the community, to prevent the uptake of smoking and support smoking cessation. The regional projects have supports to assist with best practice approaches and outcome measurement. Reducing exposure to SHS through supporting smoke-free environments is one of five nationally consistent performance indicators for organisations receiving TIS regional grant funding.
Various state/territory initiatives are in place relating to environmental tobacco smoke. For example, since 2008, in WA Tackling Smoking became a key area of initiative of the National Partnership Agreement on Closing the Gap in Indigenous Health outcomes. The development of the Midwest Region Wide Tobacco Strategy and Campaign project saw an integration of different intervention approaches, including: regulatory, structural, participative and enhancement. The multi-faceted promotional campaign used intervention approaches that included radio, newspaper, community events and the distribution of promotional materials.
Results from a short-term evaluation indicated early success and an increase in calls to the Aboriginal Quitline following the campaign. Culturally focused awareness campaigns have been shown to be effective strategies for improving the awareness of reducing the instances of SHS in the home (Maksimovic et al, 2015).