3.16 Access to after-hours primary health care
Page content
Why is it important?
‘After-hours’ refers to services provided on Sundays, before 8 am and/or after 12 pm on a Saturday, or at any time other than 8 am to 6 pm on weekdays. An important component of comprehensive primary health care services is the capacity for patients to access services after hours. In the absence of after-hours primary health care, patients with more urgent needs may delay seeking care.
It is often preferable for after-hours primary care to be provided by a patient’s usual GP, as they are more likely to know about the patient’s condition and history, and be able to make an informed judgement about the treatment required. Many patients are provided with after-hours primary care services by their regular GP or at their usual health service through extended hours clinics, on-call arrangements, the provision of home visits, and cooperative arrangements that involve GPs from several practices participating in a shared roster system.
As this is not always possible, a number of other after-hours primary care arrangements exist. These include medical deputising services (where GPs contract another service to provide after-hours services on their behalf), dedicated after-hours services (GP and/or nurse-led clinics that only open during the after-hours period) and telephone triage and advice services (which involve telephone based nurses and/or GPs providing advice and directing people to the most appropriate point of care). Many patients also attend emergency departments during the after-hours period.
The Medicare Benefits Schedule (MBS) includes after-hours items that provide increased benefit rates to medical practitioners. Rates are highest for urgent after-hours consultations where practitioners are required to provide a home visit, or return to the clinic specifically for that consultation.
Findings
Self-reported data from the 2012–13 Health Survey indicate 9% of Indigenous Australians living in non-remote areas reported accessing a doctor outside normal business hours in the previous 12 months.
According to 2015–16 Medicare data on MBS services claimed for after-hours care items, there were around 295,000 after-hours services provided to Indigenous Australians, representing 2.6% of all services (note these data may double-count after-hours care provided in selected emergency departments). After adjusting for the age differences in the two populations, the Indigenous rate was 390 per 1,000 population compared with 474 per 1,000 population for non-Indigenous Australians.
For Aboriginal and Torres Strait Islander peoples, claims for after-hours services ranged from 169 per 1,000 population in remote areas to 656 per 1,000 in major cities. Rates were lowest in the NT (155 per 1,000) and highest in SA (727 per 1,000). Indigenous rates were 1.5 times as high as non-Indigenous rates in very remote areas and only 34% as high in the NT.
From GP survey data (2010–15) it is estimated that 84% of GP encounters for Indigenous patients were with practices that had after-hours care arrangements in place (compared with 96% for other Australian patients).
In the 2014–15 Online Services Report 49% of Commonwealth-funded Indigenous primary health care organisations provided after-hours services (AIHW, 2016o). The main types of services provided after hours were transport (66%), followed by treatment of injury (61%), diagnosis and treatment of infectious illness/disease (54%), and social and emotional wellbeing/mental health/counselling services (46%). Other services provided include: diagnosis and treatment of chronic illness/disease (41%), antenatal care (36%), care in police station/lock-up (34%), maternal and childcare (25%), and substance use/drug and alcohol programs (17%).
Data on services provided by emergency departments are limited to large public hospitals, mainly located in major cities. In these hospitals, in the period 2014–15 to 2015–16, there were about 875,300 emergency department presentations by Aboriginal and Torres Strait Islander patients, representing 6% of all presentations. Around 59% (513,600) of these episodes occurred after hours. This proportion was similar for non-Indigenous patients (56%). For Aboriginal and Torres Strait Islander patients, around 55% (281,700) of emergency department presentations provided after-hours were classified as semi-urgent or non-urgent (triage categories 4 and 5) as were 50% of non-Indigenous after-hours emergency department episodes of care.
Figures
Figure 3.16-1
Age-standardised rate of MBS services claimed for after-hours care, by Indigenous status and remoteness, 2015–16
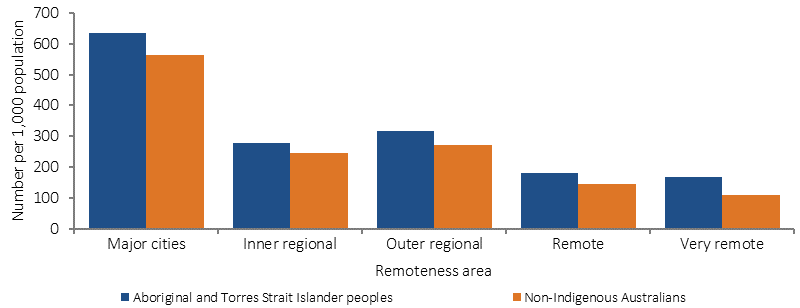
Source: Medical Benefits Division, Department of Health
Figure 3.16-2
Age-standardised rate of MBS services claimed for after-hours care, by Indigenous status and state/territory, 2015–16
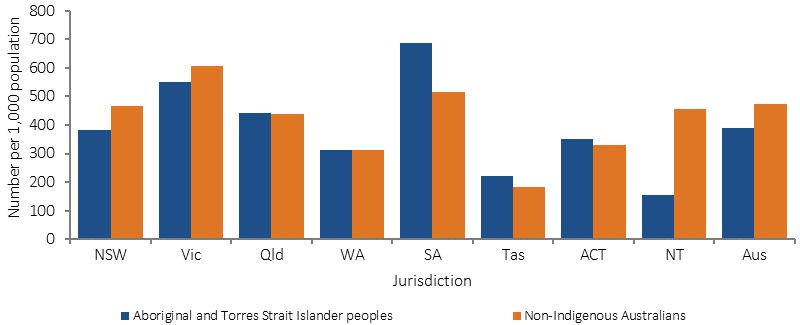
Source: Medical Benefits Division, Department of Health
Figure 3.16-3
Rate of GP encounters, by whether the GP has after‑hours arrangements in place, by Indigenous status of the patient, April 2010–March 2015
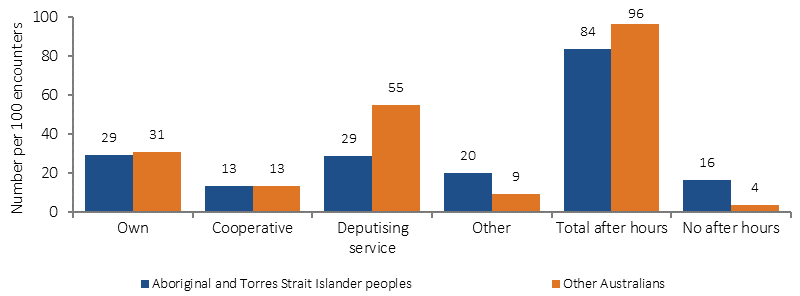
Source: Family Medicine Research Centre, University of Sydney analysis of BEACH data
Figure 3.16-4
Non-admitted patient emergency care episodes for triage categories 4 (semi-urgent) and 5 (non-urgent) by time of day and Indigenous status, July 2014–June 2016
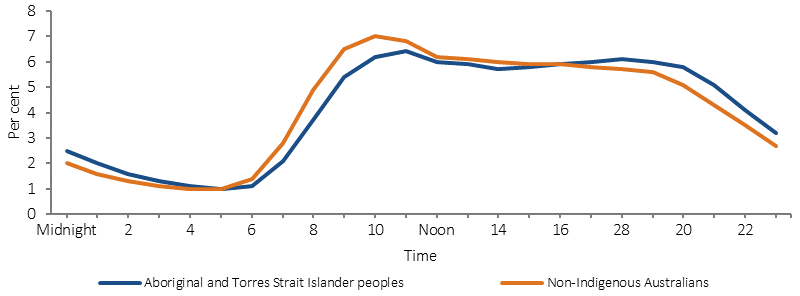
Note: Data are limited to public hospitals, mainly in major cities classified as principal referral, specialist women’s and children’s hospitals or large hospitals.
Source: AIHW analysis of National Non-admitted Patient Emergency Department Care Database
Table 3.16-1
Emergency Department presentations after-hours, by Indigenous status, July 2014–June 2016
| Time of presentation | Number | Percent | ||
|---|---|---|---|---|
| Indigenous | Non-Indigenous | Indigenous | Non-Indigenous | |
| All emergency department presentations | ||||
| On Sundays | 130,543 | 2,105,451 | 15 | 15 |
| Before 8am or after 12pm on Saturday | 103,574 | 1,554,515 | 12 | 11 |
| Before 8am or after 6pm on a weekday | 284,318 | 4,098,874 | 32 | 30 |
| Total after hours | 518,435 | 7,758,840 | 59 | 56 |
| Not after hours | 365,270 | 6,100,229 | 41 | 44 |
| Total | 883,705 | 13,859,069 | 100 | 100 |
| Semi-urgent or non-urgent (triage category 4 and 5) emergency department presentations | ||||
| On Sundays | 76,243 | 1,134,573 | 15 | 16 |
| Before 8am or after 12pm on Saturday | 57,580 | 794,372 | 12 | 11 |
| Before 8am or after 6pm on a weekday | 150,496 | 1,960,792 | 30 | 27 |
| Total after hours | 284,319 | 3,889,737 | 57 | 54 |
| Not after hours | 214,290 | 3,260,971 | 43 | 46 |
| Total | 498,609 | 7,150,708 | 100 | 100 |
| Proportion of all after hours presentations | 55 | 50 | ||
Note: These data are limited to large public hospitals mainly located in major cities.
Source: AIHW analysis of National Non-admitted Patient Emergency Department Care Database
Implications
Aboriginal and Torres Strait Islander peoples have a lower rate of MBS after-hours services claimed than non-Indigenous Australians (rate ratio of 0.8). Rates were particularly low in remote and very remote areas for Indigenous and non-Indigenous Australians and the largest gap was in the NT (rate ratio of 0.3). Note: not all care delivered through Indigenous primary health care services can be claimed through Medicare.
While Indigenous Australians make up 3% of the population, they represent 6% of emergency department presentations in hospitals for which data are collected. Over half of these presentations occurred after-hours. A better understanding is required of the needs of Aboriginal and Torres Strait Islander peoples for health services after-hours, and the best ways of providing coverage.
Following the Review of after-hours primary health care, new After-Hours Primary Health Care arrangements were implemented on 1 July 2015 and include:
- a new Practice Incentives Program (PIP) after-hours incentive payment available to eligible accredited general practices registered for the PIP
- funding to Primary Health Networks (PHNs) to support locally tailored after-hours services
- the new after-hours GP advice and support line to better support all Australians who do not have access to face to face GP services in the after-hours period.