1.09 Diabetes
Page content
Why is it important?
Diabetes is a long-term chronic condition where blood glucose levels become too high because the body produces little or no insulin, or cannot use insulin properly. Over many years, high blood glucose levels can damage various parts of the body, especially the heart and blood vessels, eyes, kidneys and nerves, resulting in permanent disability, mental health problems, reduced quality of life and premature death (Burrow & Ride, 2016; AIHW, 2016f). High blood glucose levels cause complications for both the mother and baby during pregnancy.
The most common form of diabetes is Type 2, which accounted for 85% of all diabetes in Australia in 2014–15 (ABS, 2015b). Type 2 diabetes is a significant contributor to morbidity and mortality for Indigenous Australians. It is more common in people who are physically inactive, have a poor diet, and are overweight or obese. Heredity, low birthweight, intra-uterine factors and excessive alcohol consumption are also associated with increased risk (Burrow & Ride, 2016). Type 1 diabetes is a lifelong autoimmune disease requiring management with insulin to ensure blood glucose levels remain within a safe range. In 2005–13, Indigenous Australians had a lower incidence of Type 1 diabetes (7 per 100,000) than non-Indigenous Australians (10 per 100,000) (AIHW, 2015c).
Findings
Diabetes was responsible for 4.1% of the Indigenous burden of disease in 2011 (AIHW, 2016f). Diabetes accounted for 8% of the health gap between Indigenous and non-Indigenous females, and 7% of the gap between males. High body mass (64% of burden) and physical inactivity (36% of burden) were key risk factors for diabetes. Most diabetes burden for Indigenous Australians was due to early death (68%). Between 2003 and 2011 there was a small decline (10%) for diabetes, largely driven by declines in fatal burden which outweighed the increase observed in non-fatal burden. Disease burden for Indigenous Australians due to diabetes was greater in remote areas and for those with poor socio-economic status.
The 2012–13 Health Survey included blood tests for measuring diabetes prevalence (ABS, 2014e). In 2012–13, 11% of Indigenous Australians aged 18 years and over had diabetes. After adjusting for age differences in the two populations, this was more than 3 times as high as for non-Indigenous Australians. This comprised 9.6% of Indigenous adults with known diabetes and 1.5% with diabetes newly diagnosed by the blood test results, suggesting that approximately 14% of cases of diabetes were previously undiagnosed. Of non-Indigenous adults with diabetes, 18% were previously undiagnosed . While the total diabetes rate for Indigenous adults was 3 times the non-Indigenous rate, the rate ratio for previously undiagnosed diabetes was 2 times. In addition, 5% of Indigenous Australians had blood test results showing impaired fasting plasma glucose, which means they were at high risk of developing diabetes, 1.8 times the non-Indigenous rate. Of those Indigenous adults with known diabetes, 61% had blood test results suggesting the condition was not being managed effectively. This was 1.4 times as high as for non-Indigenous Australians (44%). Half (53%) of Indigenous Australians with diabetes also had signs of chronic kidney disease (see measure 1.10).
Measured rates of diabetes for Indigenous adults were more than double in remote areas (21%) compared with non-remote areas (9%). Newly diagnosed diabetes was 5 times as high in remote as non-remote areas (4.8% compared with 0.9%). Rates of diabetes were highest in the NT (19%) and lowest in Qld (8%). Indigenous men and women had similar rates of diabetes (10% compared with 12%). Among Indigenous Australians, diabetes problems started in younger age groups than for non-Indigenous Australians. Higher rates of diabetes were evident from 35 years onwards and by 55 years and over, more than one-third of Indigenous Australians had diabetes.
There was a statistically significant relationship between the prevalence of diabetes and selected social determinants of health and risk factors such as socio-economic status, educational attainment, weight, and blood pressure.
In 2006–11, Indigenous children aged 10–14 years were 8 times as likely to have Type 2 diabetes as non-Indigenous children (AIHW, 2014d). Between 1990–2012 in WA, mean incidence of Type 2 diabetes in Indigenous children was 21 times the rate for non-Indigenous children (Haynes et al. 2016).
In 2005–07, Aboriginal and Torres Strait Islander mothers were more likely to experience pre-existing diabetes affecting pregnancy (3 to 4 times the non-Indigenous rate) and to develop gestational diabetes mellitus (GDM) (twice the non-Indigenous rate). Indigenous mothers with pre-existing diabetes were more likely to deliver pre-term (32%), compared with Indigenous mothers with GDM (14%) and Indigenous mothers without diabetes (13%) (AIHW, 2010d). Of Indigenous Australians in non-remote areas self-reporting diabetes, 69% had a blood test to check for diabetes control in the last 12 months and 68% had their feet checked in the last 12 months. In addition, 30% of Indigenous Australians with diabetes in non-remote and remote areas combined were using insulin, 64% were taking medicine/tablets and 80% had taken lifestyle action relating to diet, weight loss and exercise.
GP survey data (2010–15) showed around 5% of all problems managed by GPs among Indigenous patients were for diabetes, with Type 2 diabetes accounting for 92% of all diabetes problems managed. After adjusting for differences in the age structure of the two populations, GPs managed diabetes problems for Indigenous Australians at nearly 3 times the rate for other Australians. In the two years to June 2015, the Indigenous hospitalisation rate for diabetes was 4.2 times the non-Indigenous rate, with the gap increasing with age. Around 61% of hospitalisations for diabetes among Indigenous Australians were for Type 2 diabetes, 18% for Type 1 diabetes and a further 19% for diabetes during pregnancy. Hospitalisation rates were higher among those living in remote and very remote areas (10 per 1,000) than those in inner regional areas and major cities (4 and 5 per 1,000 respectively). Complications of diabetes such as lower limb amputations were also more common among Indigenous Australians than non-Indigenous Australians (Burrow & Ride, 2016; Rodrigues et al, 2016).
During the period 2011–15, 8% of Indigenous deaths were due to diabetes, and death rates from diabetes were 6 times the non-Indigenous rate. Diabetes was the second leading cause of the gap in death rates behind circulatory disease. There has been no decrease in death rates from diabetes for Indigenous Australians over the last 17 years. Diabetes does not often lead directly to death so complications associated with it are often listed as the cause of death (AIHW, 2014g). In 2011–15, in NSW, Qld, WA, SA and the NT there were 2,559 Indigenous deaths where diabetes was listed as an associated cause of death.
Figures
Figure 1.09-1
Proportion of Indigenous adults with diabetes by remoteness, 2012–13
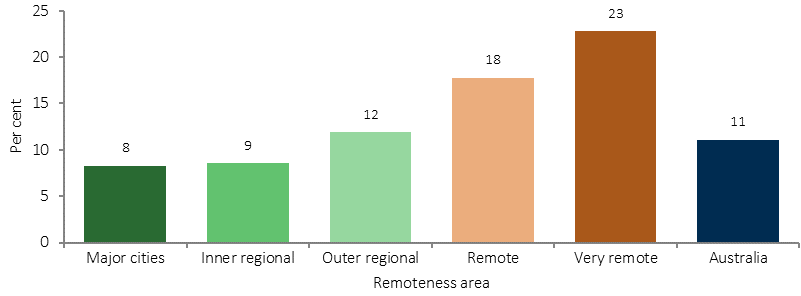
Source: ABS analysis of 2012–13 AATSIHS
Figure 1.09-2
Proportion of Indigenous Australians with diabetes by selected jurisdictions, 2012–13
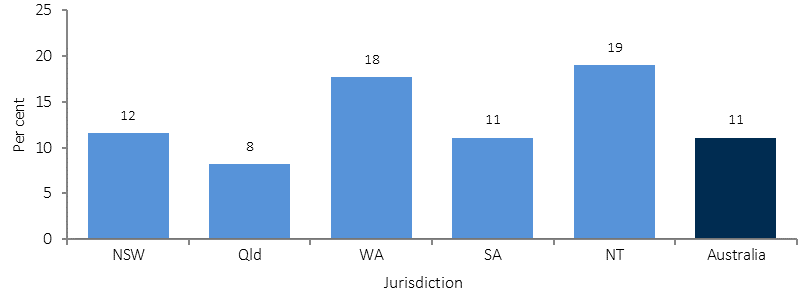
Source: ABS analysis of 2012–13 AATSIHS
Figure 1.09-3
Proportion of adults with diabetes, by Indigenous status and age, 2012–13
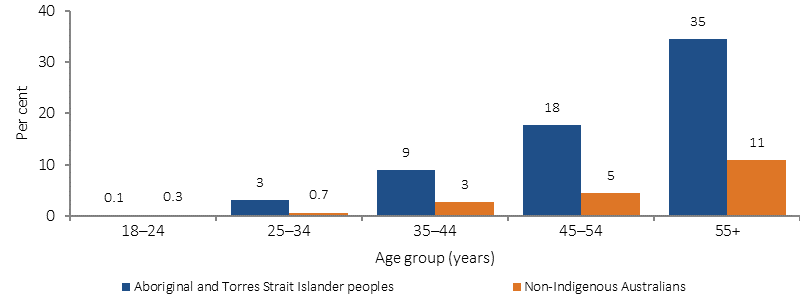
Source: ABS analysis of 2012–13 AATSIHS
Figure 1.09-4
Age-specific hospitalisation rates for diabetes, by Indigenous status, July 2013–June 2015
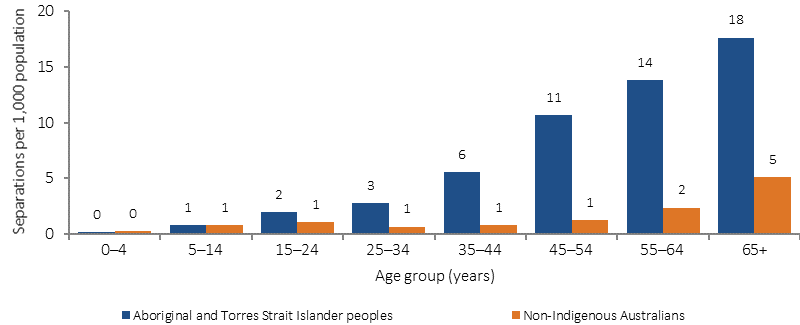
Source: AIHW analysis of National Hospital Morbidity Database
Implications
Diabetes incidence, hospitalisations and deaths are more common among Indigenous Australians than other Australians. Challenges for decision makers include maintaining a policy emphasis on primary prevention (early detection, prenatal care, nutrition, physical activity, smoking, alcohol and post-partum screening (Chamberlain et al, 2015; Rankin et al, 2016). There are also challenges in implementing strategies to achieve effective secondary prevention (such as blood sugar control; eye and feet checks; and appropriate acute care to treat serious complications as they arise).
All the goals of the Australian National Diabetes Strategy 2016–2020 are applicable to Indigenous Australians however Goal 5 has potential areas of action which specifically aim to reduce the impact of diabetes among Indigenous Australians.
The Indigenous Australians’ Health Program (IAHP) focuses on the prevention, early detection, and management of chronic disease, including diabetes, through expanded access to and coordination of comprehensive primary health care. The Quality Assurance for Aboriginal and Torres Strait Islander Medical Services (QAAMS) Pathology Program funded since 1999, aims to supports on-site diabetes-related pathology testing. Results are available in 6 minutes, enabling patients to receive their results and more comprehensive advice and treatment plans in a single visit to the health service. Funding has also been provided from the IAHP for 2016–17 to 2018–19 to provide retinal cameras and train health professionals to use them. In November 2016, two new items were listed on the MBS covering testing for diabetic retinopathy using a non-mydriatic retinal camera and annual checks for Indigenous Australians. Funding is also provided for incentive payments for improved chronic disease management, and for cheaper medicines through the PBS.
The National Diabetes Services Scheme aims to ensure people with diabetes have access to subsidised products and support services to help them self-manage their condition. A trial of pharmacy-based screening and referral for diabetes will commence in 2016.
Various state/territory initiatives are in place. For example, in Qld, $27m funding over 4 years has been committed to help tackle diabetes and other chronic diseases. Indigenous Queenslanders are one of the priority groups identified.
An NT multivariate study of Indigenous diabetes patients found that those who had an adequate level of PHC visits were likely to have a lower level of hospitalisations than those with fewer PHC visits, other things being equal (Zhao et al, 2015b). A study of Indigenous Australians with diabetes living in remote NT communities found that those who visited primary care 2–11 times per year had lower rates of death and hospitalisation than those who visited less than twice a year. Preventing one hospitalisation for diabetes was cheaper ($248 for those with medium use, $739 for complicated cases) than the cost of one hospitalisation ($2,915) (Thomas, SL, 2014).