1.06 Acute rheumatic fever and rheumatic heart disease
Page content
Why is it important?
Acute rheumatic fever (ARF) is a disease caused by an autoimmune reaction to an infection with the bacterium group A streptococcus (GAS). ARF is a short illness, but can result in permanent damage to the heart—rheumatic heart disease (RHD). A person who has had ARF once is susceptible to repeated episodes, which can increase the risk of RHD. Following an initial diagnosis of ARF, patients require long-term treatment, including long-term antibiotic treatment to avoid further infections that may damage the heart (RHD et al, 2012; AIHW, 2013b). Heart surgery may be required to repair heart valve damage resulting from RHD.
ARF and RHD are associated with environmental factors such as poverty and poor living conditions. ARF and RHD are now rare diseases in populations with good living conditions and easy access to quality medical care (He et al, 2016). Aboriginal and Torres Strait Islander peoples will remain at risk of ARF/RHD while socio-economic disadvantage and barriers to accessing health care persist.
Rheumatic Heart Disease Control Programme registers have been established in the NT, Qld and WA, and more recently in SA (currently under development). The NT RHD register has been operating in the Top End since 1997 and in Central Australia since 2001 and currently provides the strongest source of trend data on ARF and RHD. Comparisons between jurisdictions should not be made because registers are at different stages of coverage and completion. A number of smaller, geographically limited studies have also been conducted.
Findings
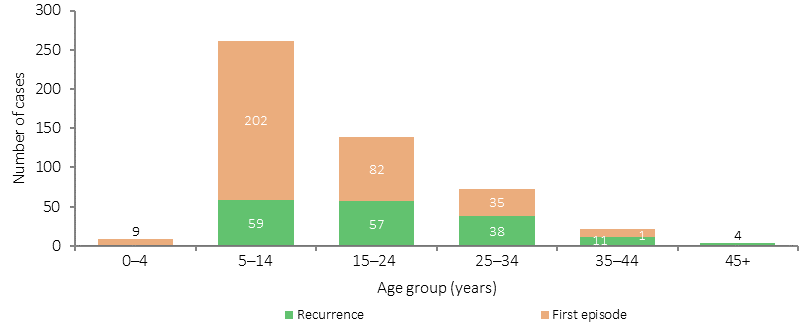
Acute rheumatic fever
In the period 2011–15, there were 1,204 new or recurrent cases of ARF in the NT, WA, Qld and SA combined (SA data is for 2013–15 only). The majority (approximately 94%, 1,132 cases) were for Aboriginal and Torres Strait Islander peoples. Based on data from the NT, WA and Qld combined, ARF is largely restricted to children and young adults: among Aboriginal and Torres Strait Islander peoples, 55% of cases occurred in children aged 0–14 years, with a further 26% in the 15–24 years age group. In the NT, most (67%) were new cases, while 33% were recurrent cases. Breakdowns by age are not currently available for SA.
Recorded rates of ARF for Indigenous Australians were 1.4 per 1,000 in the NT, 0.7 per 1,000 in WA and 0.3 per 1,000 in SA and Qld. In the NT, the rate has more than doubled between 2006 and 2015.
Rheumatic heart disease
In December 2015, there were 1,637 Aboriginal and Torres Strait Islander people recorded as having RHD in the NT, 985 in Qld, 378 in WA, and 129 in SA. The prevalence rate of RHD for Indigenous Australians was 22.1 per 1,000 in the NT, 4.7 per 1,000 in Qld, 3.9 per 1,000 in WA and 3.1 per 1,000 in SA. Females comprised 66% of Indigenous Australians in the NT with RHD. The prevalence of RHD was 37 times as high among Indigenous Australians as it was among other residents of the NT, 169 times higher for Indigenous Australians in Qld, and 630 times higher in WA.
A study conducted between 2006 and 2010 found large differences in RHD prevalence rates among Indigenous children in Northern Australia, ranging from 15 per 1,000 in the Top End of the NT to 4.7 per 1,000 in Far North Qld. More than half of the definite RHD cases detected were new cases, and the findings suggest that between 4 and 8 per 1,000 Indigenous children have undetected RHD. Regions with higher prevalence rates were associated with lower socio-economic conditions (Roberts et al. 2015).
Between 2006 and 2015 there was a 24% non-significant decline in new registrations of RHD among Indigenous Australians in the NT. There was an increase in new registrations of RHD in WA between 2010 and 2015, though this is likely to be at least in part due to improved diagnosis and increased registration.
An audit of control programmes in far North Queensland and the Kimberley region of WA found that 1 in 5 patients with RHD had been prescribed an anti-coagulant, 55% had received a specialist review within recommended timeframes, 61% had a timely echocardiogram and 22% had undergone valve surgery. Of patients who were recommended benzathine penicillin secondary prophylaxis, only 18% received more than 80% of scheduled doses in the 12 months prior (Remond et al, 2013).
Indigenous Australians were 5 times as likely to die from rheumatic heart disease as non-Indigenous Australians (6.4 per 100,000 compared with 1.4 per 100,000). A data linkage study in the NT found that mortality was 6.6 times higher among Indigenous than non-Indigenous RHD patients, and that 28% of this difference was explained by renal failure and hazardous alcohol use (He et al, 2016).
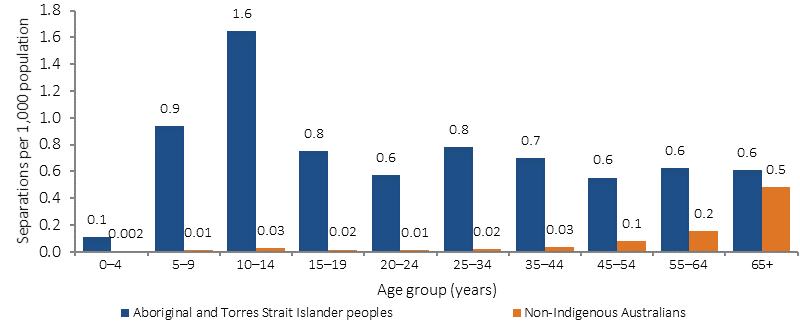
Indigenous Australians were hospitalised for ARF/RHD at rates of around 7 times that for other Australians (0.7 per 1,000 compared with 0.1 per 1,000 for non-Indigenous Australians in the period 2013–14 to 2014–15). Rates were highest in the NT (3.0 per 1,000) and lowest in NSW (0.2 per 1,000). Hospitalisations for Indigenous Australians were highest in the 10–14 year age group whereas for non-Indigenous Australians rates increased with age and were highest in the 65 years and over group. Indigenous Australians hospitalised for ARF/RHD were less likely than other Australians to have had at least one heart valve procedure performed (26% compared with 44%).
Figures
Figure 1.06-1
Acute rheumatic fever incidence, Northern Territory 2011–15
Source: AIHW analysis of Northern Territory Rheumatic Heart Disease Program Register
Figure 1.06-2
Hospitalisations with a principal diagnosis of acute rheumatic fever or rheumatic heart disease, by age and Indigenous status, July 2013–June 2015
Source: AIHW analysis of National Hospital Morbidity Database
Implications
Rates of ARF and RHD among Indigenous Australians are among the highest in the world and large inequalities exist between Indigenous and other Australians (AIHW, 2013b). Interventions that focus on improving housing, socio-economic circumstances and health care are important for preventing and managing these conditions. Improved access to appropriate treatment for GAS infections such as throat and skin infections are likely to reduce the rate of ARF. More research is needed on the association between GAS skin infections and ARF as the findings of studies to date have not been definite (RHD et al, 2012; May et al, 2016; Carapetis et al, 2007).
A study in the NT found high progression rates to RHD following the first year after ARF diagnosis, particularly among Indigenous Australians in remote areas, and those with comorbidities (He et al, 2016). Development of complications is also more likely in the first year after diagnosis. These findings suggest limitations to secondary prevention. This study also found residual disparities in Indigenous RHD survival after accounting for comorbidities (such as renal failure and alcohol use). May and others (2016) recommend preventative measures such as monitoring GAS diseases, the development of a GAS vaccine, long-acting penicillins, and note the importance of improvements in social determinants for Indigenous Australians, along with better access to health care and improved housing.
Even so, secondary prevention and treatment of ARF/RHD are essential, through the implementation of disease registers and control programmes, education of patients and their families, treatment with penicillin prophylaxis, and regular clinical review and access to specialists and hospital care (Chamberlain-Salaun et al, 2016). It has been suggested that the introduction of specialist ARF/RHD nurse practitioners in Australia could help to improve service delivery and patient outcomes (RHD & MSHR, 2015).
The May 2014 Better Cardiac Care for Aboriginal and Torres Strait Islander People Post Forum Report identifies strengthening the diagnosis, notification and follow-up of RHD as a priority for action by all jurisdictions. This forum was an initiative of the Australian Health Ministers’ Advisory Council.
The second Better Cardiac Care Measures for Aboriginal and Torres Strait Islander People report shows progress against 11 of the 21 recommended indicators for which updated data were available, including three of the four indicators for RHD (AIHW, 2016a).
RHD registers are a central element of secondary disease prevention programs to prevent recurrence of ARF and reduce the occurrence or severity of RHD. Control programs improve case detection, and are the most effective way of improving compliance to treatment and supporting clinical follow-up of people with RHD.
The Australian Government’s Rheumatic Fever Strategy (RFS) provides funding for register and control programs in the NT, WA, Qld and SA, and funding for a National Coordination Unit, RHD Australia.
Under the RFS, funding is provided to help improve the detection and diagnosis of ARF and RHD, and improve access to the antibiotic injections that prevent repeated attacks of ARF. The RFS provides funding of $14.7 million over five years (2012–13 to 2016–17) for state-based register and control programs, and $4.4 million over five years (2012–13 to 2016–17) for the National Coordination Unit (NCU). The NCU supports the state-based programs to operate in accordance with best practice clinical guidelines; develops national education, training and self-management resources; and is developing a performance monitoring system to improve the collection of data and reporting on incidence and prevalence.
The Indigenous Australians’ Health Programme focuses on the prevention, early detection and management of chronic disease, including circulatory diseases such as ARF/RHD (see Policies and Strategies for more details).
In addition to the activities funded under the IAHP, the Australian Government provides funding for GP health assessments for Aboriginal and Torres Strait Islander people under the MBS, which includes follow-on care. Funding is also provided for incentive payments for improved chronic disease management, and for cheaper medicines through the PBS.
Further research is also important. The END RHD CRE is a Centre for Research Excellence which has been established to develop a comprehensive, evidence-based strategy for tackling RHD. The CRE focuses on better measurement, prevention and treatment of RHD, and collaboration across relevant medical and research bodies. NHMRC has provided funding for the CRE for five years from May 2015.
ARF and RHD are uncommon diseases in most places in Australia, so the majority of health professionals have poor awareness and knowledge about these preventable diseases. Maintaining high levels of secondary prophylaxis with regular penicillin injections can reduce recurrences and progression to RHD. Following the integration of an indicator to monitor secondary prophylaxis rates into the Northern Territory Aboriginal Health Key Performance Indicators system, there has been significant improvement in coverage rates.
The South Australian RHD program and register supports primary health care services across SA in the management of their patients with ARF and RHD, in particular with the delivery of four weekly preventative antibiotic injections, which are required for a minimum of ten years. Since the Program’s inception in 2012, there has been a steady increase in the number of people with ARF and/or RHD who are adhering to their treatment regime. Data from the SA register shows that in 2012 the average adherence to these injections was 58%, while at the end of 2015 it was 80%.