3.04 Early detection and early treatment
Page content
Why is it important?
Early detection is the discovery of a disease or condition at an early stage of its development or onset, usually before symptoms occur. Early detection may occur for individual patients, where clinically indicated, or for targeted populations through screening programmes. Early detection and treatment programmes are most effective when there are systematic approaches to ensuring assessment and screening occurs regularly and at recommended intervals. In Australia, primary health care providers, including Aboriginal and Torres Strait Islander health services and GPs, have a key role.
Screening programmes are designed to detect cancer early (breast and bowel) or prevent its occurrence in the first place (bowel and cervical). National programmes for breast and cervical screening were implemented in Australia in the early 1990s. The National Cervical Screening Program (NCSP) currently recommends regular screening for women aged 18–69 years. BreastScreen Australia recommends two-yearly screening for women aged 50–74 years. The National Bowel Cancer Screening Program (NBCSP) began in 2006 and is working towards biennial screening for those aged 50 to 74 years. Research suggests that biennial bowel cancer screening can save up to 500 lives annually (Pignone et al, 2011).
While cancer mortality is higher among Indigenous Australians (see measure 1.08), participation rates in the NBCSP and BreastScreen Australia have been lower than non-Indigenous rates (AIHW, 2016w; AIHW, 2014a) and Indigenous women appear to be under-screened in the NCSP (AIHW, 2016t; Whop et al, 2016).
Findings
Health checks
Medicare Benefits Schedule (MBS) health assessment items for Aboriginal and Torres Strait Islander peoples aim to encourage early detection, diagnosis and intervention for common and treatable conditions that cause morbidity and early mortality. Health assessment items for Indigenous Australians aged 55 years and over were introduced in 1999, for those aged 15–54 years in 2004, and in 2006 for 0–14 year-olds. In 2009–10, measures to increase take-up of health assessments by those aged 15 and over were introduced.
Trend analysis shows a statistically significant increase in health assessments for all ages between 2009–10 and 2015–16 (the rate has more than tripled). There has been acceleration in the rate of change since 2009–10 (annual average change of 33 per 1,000, compared with 27 per 1,000 for the period 2006–07 to 2015–16).
In 2015–16, around 63,800 health assessments were undertaken for children aged 0–14 years, representing around 26% of children in the target group. There were about 103,600 health assessments provided for Indigenous Australians aged 15–54 years (25% of this population) and 29,400 for those aged 55 years and over (representing 38% of this population). Health assessments through Medicare are also available to all Australians aged 75 years and over, with 33% of this population having an assessment in 2015–16.
In Commonwealth-funded Indigenous primary health care organisations, 33% of Indigenous children aged 0–4 years (who were regular clients) had received an MBS health assessment in the 12 months to May 2015. For eligible adults who are regular clients, 44% of those aged 25–54 years had received a health check in the previous 24 months as had 52% of those aged 55 years and over.
In the 2012–13 Health Survey, Indigenous Australians aged 50 years and over with no current diagnosis for diabetes were 1.2 times as likely as non-Indigenous Australians to have been tested for diabetes/high sugar levels in the last three years (67% compared with 55%).
Cancer screening
In the latest BreastScreen Australia data, which covers the two calendar years 2013–14, 37% of Indigenous Australian women aged 50–69 years had been screened (nearly 16,000 women) compared with 54% of non-Indigenous women (age-standardised).
Participation ranged from 28% in the NT to 47% in Qld. Over the period 1999–2000 to 2013–14, there has been a 12% increase in the proportion of Indigenous women screened (and a 20% increase for non-Indigenous women). In the 2012–13 Health Survey, 79% of Indigenous women aged 50–69 years reported having ever had a mammogram.
Based on 2014–15 Social Survey self-reported data, 55% of Aboriginal and Torres Strait Islander women aged 20–69 years had a pap test at least every two years. Women living in major cities were more likely to report two-yearly screening than those living in very remote areas (53% and 51% respectively).
In 2015, Commonwealth-funded Indigenous primary health care organisations reported that 30% of regular female clients had a cervical screening in the previous 2 years, 39% in the previous 3 years and 48% in the previous 5 years. Proportions were highest in the NT and very remote areas (66% and 62% respectively for those screened in the last 5 years).
For all Australian women aged 20–69, 57% were recorded in the national cervical screening register in 2014–15 (AIHW, 2016r).
In 2014, around 487,700 Australians participated in the NBCSP, with just under 3,900 (0.8%) identifying as Indigenous. Participants recorded as Indigenous were more likely to receive a positive (i.e. potentially abnormal) test result than non-Indigenous participants (11% and 7% respectively). Yet Indigenous participants with a positive result had lower rates of follow-up colonoscopy (59% compared with 74%) and a longer median time between a positive screen and assessment (83 days compared with 54) (AIHW, 2016q).
In the 2012–13 Health Survey, for those aged 50–74 years, 18% of Indigenous males and 11% of Indigenous females reported having ever participated in bowel cancer screening tests. For Indigenous males aged 50 years and over, 64% reported having ever been tested for prostate cancer in 2012–13.
Figures
Figure 3.04-1
MBS health assessment rates, by selected age groups, Indigenous Australians, 2006–07 to 2015–16
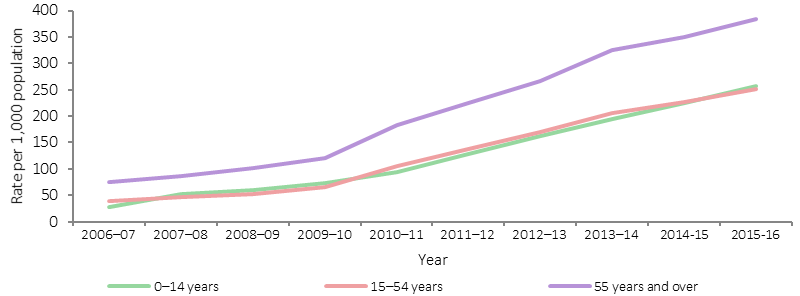
Source: AIHW analysis of Medicare Australia data
Figure 3.04-2
Participation rates for BreastScreen Australia, women aged 50–69 years, by Indigenous status, 1999–2000 to 2013–14
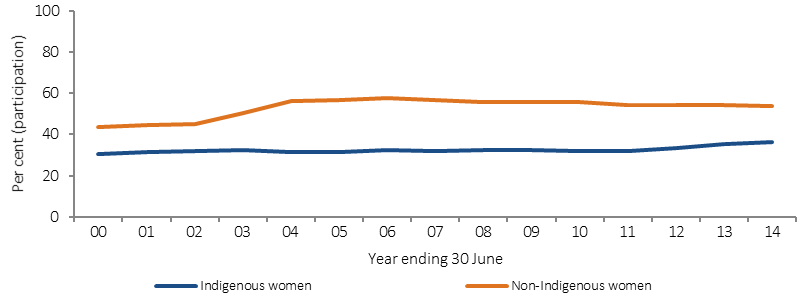
Source: AIHW analysis of BreastScreen Australia data
Figure 3.04-3
Proportion of Indigenous women aged 20–69 years reporting having at least 2 yearly pap test, by remoteness, 2012–13
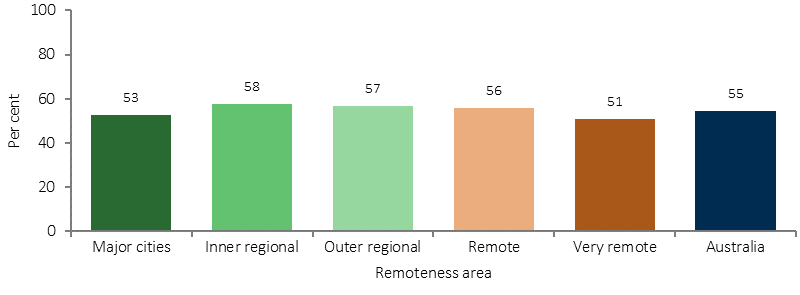
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Table 3.04-1
Summary of NBCSP screening, results and assessments, people aged 50–74, by Indigenous status, 2014
| Indigenous | Non-Indigenous | |
|---|---|---|
| Numbers | ||
| Screened | 3,888 | 473,702 |
| Positive FOBT result | 407 | 33,007 |
| Diagnostic assessment (colonoscopy) | 239 | 24,438 |
| Rates (%) | ||
| FOBT positivity rate | 10.5 | 7 |
| Diagnostic assessment rate | 58.7 | 74 |
| Time between positive screen and assessment (days) | ||
| Median | 83 | 54 |
| 90th percentile | 196 | 154 |
Source: National Bowel Cancer ScreeningProgram Register as at 31 December 2015
Implications
Early detection and early treatment through primary health care has significant benefits for those at risk of disease. Identification of Indigenous patients is the first step in providing access to Aboriginal and Torres Strait Islander specific health initiatives, including the additional MBS, Pharmaceutical Benefits Scheme (PBS), and immunisation. Improving follow-up of abnormal clinical findings/results and access to referral services is also critical to achieving the benefits of health assessments and screening programmes (Bailie, J et al, 2014; Spurling et al, 2009; Whop et al, 2016).
The Australian Government provides GP health assessments for Aboriginal and Torres Strait Islander peoples under the MBS, along with follow-on care and incentive payments for improved chronic disease management and cheaper medicines through the PBS. The Practice Incentives Program—Indigenous Health Incentive aims to support general practices and Indigenous health services to provide better health care for Indigenous patients including identifying the Indigenous status of patients and best practice management of chronic disease.
Chronic disease strategies are included in the Implementation Plan for the National Aboriginal and Torres Strait Islander Health Plan 2013–2023 and the Indigenous Australians’ Health Programme (see Policies and Strategies section). Under the Plan, the rate of health assessments for those aged 0-4, 5-14, 15-24, and 25-54 years is being monitored. For trend analysis of these groups see the AIHW Detailed Analyses.
Given the lower Indigenous participation rates in breast, bowel and cervical cancer screening programmes, better ways of encouraging regular screening are needed (Christou et al, 2010). In the 2014–15 Budget, the Australian Government committed to accelerate the roll-out of a biennial bowel screening interval for all Australians aged 50–74 years of age from 2015 to 2020.
Three years of funding from 2016–17 has been allocated to pilot and evaluate a range of strategies to increase NBCSP participation in up to 50 Indigenous primary health care services to determine the most effective model/strategies for potential national implementation. The pilot will have screening kits offered by health professionals as an alternative to the usual direct mail approach and test different levels of implementation support and training for participating services.
Communication activities encouraging Aboriginal and Torres Strait Islander people to participate in both breast screening and bowel screening has been ongoing since 2014.
The Wirraka Maya Health Service funds primary prevention in Aboriginal communities (e.g. child health checks, hygiene sessions, ear health education, an alcohol in pregnancy intervention and development of an outreach service to surrounding communities), which has resulted in an estimated 400 child health checks and 1,000 immunisations per annum. Cancer Council Victoria’s Under Screened Recruitment Program targets Indigenous Australian participation in breast, cervical and bowel screening.
Cervical screening will remain vital for many decades as the current HPV vaccines are not effective against all types of the virus that cause cervical cancer. A barrier to reporting on cervical screening is that pathology request forms do not include provision for Indigenous status to be recorded in all jurisdictions.