3.03 Health promotion
Page content
Why is it important?
Aboriginal and Torres Strait Islander peoples currently experience higher levels of morbidity and mortality from potentially avoidable conditions than other Australians. In 2011–15, 61% of Indigenous deaths before the age of 75 years were potentially avoidable. The Indigenous avoidable mortality rate was 3 times the non-Indigenous rate (see measure 1.24). Exposures to risk through behaviours such as smoking were also higher (see Health Behaviour measures).
Health promotion is the process of enabling people to increase control over their health and its determinants, and thereby improve their health (WHO, 2005). Health promotion activities are designed to improve or protect health within social, physical, economic and political contexts. Health promotion includes public policy interventions (e.g. packaging of tobacco products, seat belt laws), information to support healthy lifestyles (e.g. smoking, alcohol and drug use, physical activity, diet), social marketing (e.g. sunscreen, safe sex) and mass media campaigns (e.g. drink-driving, road safety). Health promotion also includes empowering individuals, strengthening community capacity and addressing determinants of health.
Currently there are limited methods for measuring the nature, level, and reach of health promotion programmes and activities.
Findings
Estimating expenditure on health promotion for Indigenous Australians is difficult as it is often embedded within other funding sources and programs (e.g. funding for GPs, primary health care and mainstream health promotion activities). In 2013–14, state and territory government expenditure on public health for selected health promotion activities was estimated to be around $15 for each Indigenous Australian and $16 for each non-Indigenous Australian. In addition, expenditure for the prevention of hazardous and harmful drug use was estimated to be $5.90 per Indigenous Australian and $6.20 per non-Indigenous Australian. Australian Government funding for public health services was $120 per person for Indigenous Australians; however, this includes a broad set of activities from which health promotion could not be separated out.
In the 2012–13 Health Survey, 46% of Indigenous Australians aged 15 years and over who had consulted a doctor in the last 12 months reported discussing lifestyle issues. These included reaching a healthy weight (50%), improving diet (44%), reducing or quitting smoking (43%), increasing physical activity (30%), drinking alcohol in moderation (16%), safe sexual practices (12%) and family planning (10%).
Indigenous Australians in the NT and in remote areas were less likely to have accessed a doctor in the last 12 months and also less likely to have discussed lifestyle issues than those living in other areas. Females were more likely to have discussed lifestyle issues with a doctor than males (50% and 41% respectively), while discussions on drinking alcohol in moderation were more common for males (26%) than for females (8%).
Based on GP survey data (2010–15), 32% of all clinical and therapeutic treatments provided by GPs to Indigenous patients related to health promotion. General ‘advice/education’ accounted for 9% of all clinical and therapeutic treatments, followed by ‘advice/education treatment’ and ‘counselling/advice for nutrition and weight’ (both 6%) and ‘counselling/advice for smoking’ (3%). After adjusting for differences in the age structure of the two populations, the rate at which GPs provided counselling and advice about smoking was nearly 3 times as high, and for both alcohol and lifestyle advice almost twice as high, at encounters with Indigenous patients than other Australian patients. The total rates of GP clinical treatments relating to health promotion were slightly higher for Indigenous patients (204 per 1,000 GP encounters) than for other Australian patients (178 per 1,000 encounters).
In 2014–15, all Commonwealth-funded Indigenous primary health care organisations provided a range of health promotion programs and activities. These included immunisation services to children (81%) and to adults (79%); healthy lifestyle programs (81%), sexual health promotion (67%) and mental health promotion activities (47%). Most (89%) of these organisations also provided group activities. These included promotion of physical activity/healthy weight (73%) tobacco use treatment/prevention (56%), alcohol use treatment/prevention (40%), and living skills (such as cooking and nutrition) (61%).
Health promotion activities were also a key feature of programs run by Aboriginal and Torres Strait Islander substance-use specific services, with 76% running living skills groups, 70% running group activities on physical activity/healthy weight, 69% running men’s groups and 58% women’s groups in addition to substance-specific group activities for alcohol (81%) and tobacco (67%) treatment/prevention.
Figures
Figure 3.03-1
Types of lifestyle issues discussed with GP/health professional in last 12 months, Indigenous Australians aged 15 years and over, 2012–13
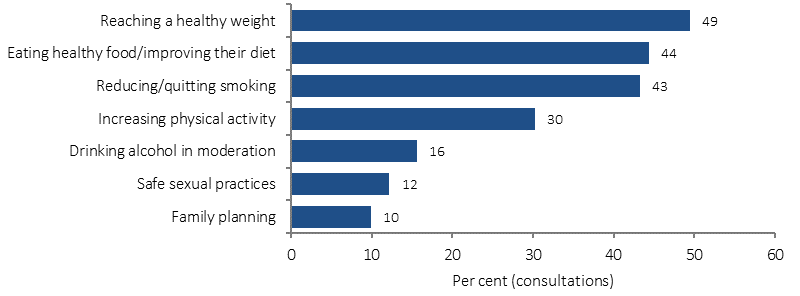
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Figure 3.03-2
Proportion of Indigenous Australians aged 15 years and over who discussed lifestyle issues with GP/health professional in last 12 months, by remoteness, 2012–13
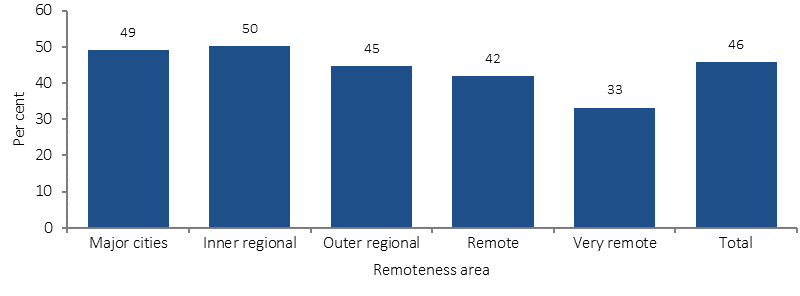
Source: ABS and AIHW analysis of 2012–13 AATSIHS
Implications
Not all health campaigns are effective. Evidence on the effectiveness of health promotion is mixed across a range of settings and disease types with some approaches more effective than others for different population groups (Liu et al, 2012; Jackson & Waters, 2005). Factors that influence health behaviour and health behaviour change among Indigenous Australians are also complex and poorly understood (Waterworth et al, 2015).
A recent literature review found that while Indigenous health promotion tools were widely available, only 15% had been evaluated, and only half of these evaluations were considered comprehensive (McCalman et al, 2014). Programmes that were more successful had allowed local communities to determine the end product by asking them what type of health promotion they would like, on what topic and how they would like it delivered (Charles, 2016; Schoen et al, 2010).
While studies can model the continued effectiveness of health promotion interventions, there is limited evidence on long-term behavioural change (Merkur et al, 2013). A small study of urban Indigenous young people found no change in behaviours but some change in knowledge and attitudes following health promotion interventions in school (Malseed et al, 2014). At the heart of health promotion is effective communication that takes into account language and world view to support people to live healthy lives (Vass et al, 2011).
Features of effective health promotion interventions for Indigenous communities include: involving local Indigenous people in design and implementation of programs; acknowledging different drivers that motivate individuals; building effective partnerships between community members and the organisations involved; cultural understanding and mechanisms for effective feedback to individuals and families; developing trusting relationships, community ownership and support for interventions (Black, 2007). Family-centred approaches across the life course have also been recommended in the prevention of chronic disease (Griew et al, 2007).
Don’t Make Smokes Your Story (Dept. of Health, 2016) is the latest phase of the National Tobacco Campaign using an empowering and positive approach to encourage quit attempts among Indigenous smokers. Break the Chain and Quit for You, Quit for Two, are part of an integrated strategy utilising mainstream mass media, local and targeted channels, digital and social media, and below the line activities.
The Australian Government’s Tackling Indigenous Smoking (TIS) programme funds regional projects to deliver a range of evidence-based activities that suit the local context and the needs of the community to prevent the uptake of smoking and support smoking cessation.
The 2016 Girls Make Your Move campaign encourages and supports young women aged 12–19 years to be more active and reinforces the benefits of an active life. Indigenous girls feature in the campaign advertising which was placed in Indigenous specific media channels.
The Health Star Rating social marketing campaign is intended to support all grocery buyers of packaged goods to make more informed nutritional choices at the point of purchase by providing easy-to-understand front-of-pack labelling. The campaign includes a specific focus on out-of-home and social media aimed at Indigenous audiences.
Targeted communication activities have been delivered to promote the BreastScreen Australia program and the National Bowel Cancer Screening Program to Aboriginal and Torres Strait Islander audiences, with the aim of increasing participation and subsequently delivering better health outcomes. Culturally specific advertising and public relations activities have been delivered.
The Foetal alcohol spectrum disorder (FASD) prevention program is an alcohol in pregnancy project in the Kimberly region run by the Ord Valley Aboriginal Health Service. The program applies innovative strategies in providing education and support of antenatal clients and their families, as well as providing regular education sessions to students in the region. The success of the program can be attributed to both community investment and ownership and the willingness of the Aboriginal community to embrace change.
Strong Spirits, Strong Minds is a media campaign that aims to prevent and/or delay the early uptake of alcohol and other drugs by young Aboriginal people in the Perth metropolitan area. The multi-faceted communication strategy includes mainstream mass communication channels to deliver Aboriginal specific messages. The project was developed from a strong cultural foundation with input from an Aboriginal youth advisory panel. Evaluation results indicate it is a highly effective and successful strategy.
‘Alive and Kicking Goals’ is a multi-award winning youth suicide prevention project based in the Kimberley region. The project aims to reduce the high suicide rate among Aboriginal and Torres Strait Islander youth through peer education workshops, one-on-one mentoring and counselling. The project is wholly owned and led by young Aboriginal women and men.
In WA, Tackling Smoking–a development of the Midwest Region Wide Tobacco Strategy and Campaign is a project that integrated different intervention approaches (e.g. regulatory, structural, participative and enhancement). The multi-faceted promotional campaign used radio, newspaper, community events and the distribution of promotional materials. Results from a short-term evaluation indicated early success and an increase in calls to the Aboriginal Quitline following the campaign.
The Aboriginal and Torres Strait Islander Smoking Cessation Program in the ACT supports a number of smoking cessation activities in the region, with an emphasis on pregnant smokers and their cohabitants.