2.19 Dietary behaviours
Page content
Why is it important?
Many of the principal causes of ill-health among Aboriginal and Torres Strait Islander peoples are nutrition-related diseases, such as heart disease, Type 2 diabetes and renal disease. While a diet high in saturated fats and refined carbohydrates increases the likelihood of developing these diseases, regular exercise and intake of fibre-rich foods, such as fruit and vegetables, can have a protective effect against disease (Wang, X et al, 2014). The National Health and Medical Research Council updated their Australian Dietary Guidelines in 2013. The guidelines specify recommendations for intake of food from the five food groups for good health, weight maintenance and the prevention of diet-related chronic diseases. They include recommendations for adequate minimum daily intake of fruit and vegetables. Recommended food consumption depends on age, and sex and life stage (e.g. pregnant, breastfeeding) (NHMRC, 2013a; ABS, 2014b).
The burden of disease study (AIHW, 2016f) attributed 9.7% of the total burden of disease in the Aboriginal and Torres Strait Islander population to 13 diet risk factors (joint effect) in 2011. Diet-related diseases are caused by combinations and interactions of environmental, behavioural, biological, social and hereditary factors. There is a substantial quantity of evidence that associates dietary excesses and imbalances with chronic disease. Of particular relevance in Indigenous communities are factors such as socio-economic status and other risk factors including insulin resistance, glucose intolerance, obesity (especially central fat deposition), hypertension, high blood triglycerides, perinatal and postnatal nutrition and childhood nutrition (NHMRC, 2000; Longstreet et al, 2008). Good maternal nutrition and healthy infant and childhood growth are fundamental to the achievement and maintenance of health throughout the life cycle. Inadequate nutrition during pregnancy is associated with low birthweight in babies (see measure 1.01).
Growth retardation among Indigenous infants after the age of 4 to 6 months has consistently been noted (Bar-Zeev et al, 2013). Australian overweight/obesity rates have also increased from 56% of the adult population in 1995 to 63% in 2014–15 (ABS, 2015b).
Findings
The latest data on dietary behaviours for Aboriginal and Torres Strait Islander peoples comes from the 2014–15 Social Survey. In 2014–15, 5% of Indigenous Australians aged 4–14 years and 4% of those aged 15 years and over reported adequate daily fruit and vegetable intake.
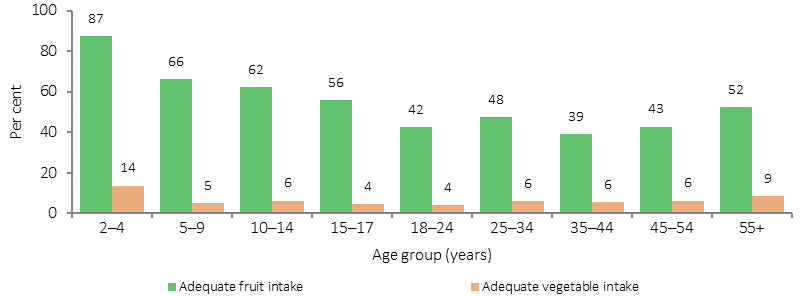
For those aged 12 years and over, 47% were eating the recommended daily intake of fruit (2 serves) and 6% the recommended daily intake of vegetables (5–6 serves). The recommendations for minimum serves of fruit and vegetables were lower for children (around half of the adult recommendations). In 2014–15, 65% of Indigenous children aged 4–14 years met the recommended fruit intake and 6% the recommended vegetable intake.
The majority of Indigenous Australians aged 12 years and over reported eating at least one serve of vegetables daily (88%) and also at least one serve of fruit (75%). Between 2012–13 and 2014–15 (in non-remote areas), there has been an increase in the proportion of Indigenous Australians aged 12 years and over meeting the recommended daily vegetable intake (4.6% to 6.1%). There has also been an increase in adequate fruit intake, from 42% in 2012–13 to 46% in 2014–15.
In 2014–15, Indigenous children aged 2-4 years had the highest proportion of adequate daily fruit (87%) and vegetable (14%) intake. Adequate daily intake of fruit and vegetables was similar for Indigenous Australians aged 12 years and over in remote and non-remote areas. A higher proportion of Indigenous females aged 12 years and over reported adequate daily fruit and vegetable intake (6%) compared with Indigenous males (2%).
Comparisons to non-Indigenous Australians are only available through the 2012–13 Health Survey. After adjusting for differences in the age structure of the two populations, Indigenous Australians aged 12 years and over were 1.4 times as likely as non-Indigenous Australians to report less than one serve of fruit daily and 1.9 times as likely to report less than one serve of vegetables. Rates of recommended levels of daily fruit and vegetable intake were lower for Indigenous Australians than for non-Indigenous Australians (ratio of 0.9 for fruit and 0.8 for vegetables).
The nutrition component of the 2012–13 Health Survey found that 41% of total daily energy reported as consumed by Indigenous Australians was from discretionary foods, that is, foods considered to be of little nutritional value and which tend to be high in saturated fats, sugars, salt and/or alcohol (compared with 35% for non-Indigenous Australians) (ABS, 2015a). Median alcohol consumption was twice as high among Indigenous consumers than non-Indigenous consumers. Indigenous children aged 2–3 years were three times as likely as non-Indigenous children aged 2–3 years to have consumed Soft drinks, and flavoured mineral waters (18% compared with 5.8%). Indigenous Australians in non-remote areas were more likely than those in remote areas to consume: fruit (49% compared with 35%) and soft drinks (39% compared with 32%); and less likely to consume meat dishes (74% in non-remote compared with 81% in remote areas). Indigenous Australians aged 2 years and over were more likely than non-Indigenous Australians to consume meat (76% compared with 69%), and snack foods (20% compared with 15%), soft drinks (37% compared with 29%); and less likely to consume vegetables (65% compared with 75%).
The 2014–15 Social Survey showed an association between dietary behaviour and other socio-economic and health characteristics. For example, Indigenous Australians aged 15 years and over who were employed were more likely than unemployed Indigenous Australians to report adequate fruit intake (48% compared with 39%).
Figures
Figure 2.19-1
Whether met guidelines for adequate intake of fruit and vegetables, Indigenous Australians, by age, 2014–15(a)(b)
(a) Based on one serve of fruit for children aged 2–8 years and two serves for persons aged 9 years and over.
(b) Based on two serves of vegetables for children aged 2–3 years, four serves for ages 4–8 years and five for persons aged 9 years and over with the exception of 18–49 year old males to eat six serves.
Source: AIHW and ABS analysis of 2014–15 NATSISSS
Figure 2.19-2
Major food group consumption by Indigenous status, persons aged 2 years and over(a), 2012–13
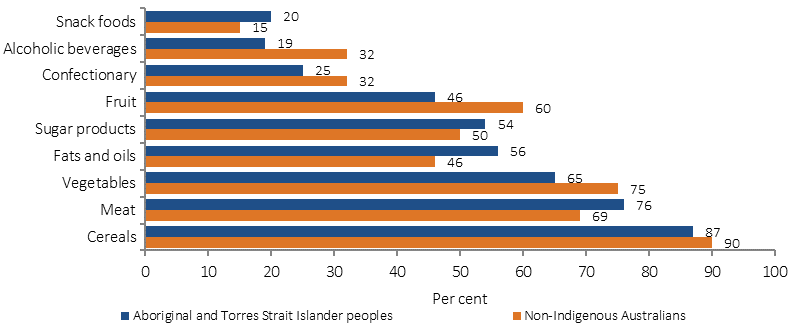
(a) Alcohol data is for persons aged 19 years and over
Source: ABS 2015
Implications
Evidence suggests that people living in poverty tend to maximise calories per dollar spent on food. Energy-dense foods rich in fats, refined starches and sugars represent the lowest-cost options, while healthy diets based on lean meats, whole grains and fresh vegetables and fruits are more costly (Drewnowski & Specter, 2004). People in vulnerable groups may therefore simultaneously be overweight or obese and experience food insecurity (AIHW, 2012a).
In 2012–13, 9% of Indigenous Australians aged 15 years and over went without food when they could not afford to buy more. Indigenous Australians were 7 times as likely as non-Indigenous Australians to go without food due to financial constraints in the previous 12 months. A person's access to a healthy diet can be influenced by a range of socio-economic, geographical and environmental factors. Food security, food access and food supply issues are of particular importance in rural and remote areas. Remote stores often have a limited range of foods, particularly perishable foods such as fresh fruit, vegetables and dairy foods, and purchase prices are usually higher (Pratt et al, 2014; Scelza, 2012; DAA, 2013). Low income combined with high food costs result in many Indigenous Australians spending a large proportion of their income on food and contributes to concerns about going without food (Brimblecombe & O’Dea, 2009).
In 2009–10, the National Aboriginal and Torres Strait Islander Nutrition Strategy and Action Plan (NATSINSAP) was evaluated to determine how effectively it was implemented and how it could be more effective and responsive to the current environment. The evaluation identified that the key achievements of NATSINSAP were in three of the seven priority action areas: food supply in remote and rural communities; disseminating and communicating good practice; and Aboriginal and Torres Strait Islander nutrition workforce. Some specific examples within these priority action areas include: the launch of the Remote Indigenous stores and takeaways resources; the development of nationally accredited nutrition training materials for Indigenous health workers; the revival of the National Nutrition Networks conference and development of an Indigenous nutrition web directory on the Australian Indigenous Health InfoNet.
The 2013 Australian Dietary Guidelines (‘the Guidelines’) provide evidence-based healthy eating advice for good health and the prevention of obesity and diet-related chronic diseases. The Guidelines apply to all population groups, including adults, children and adolescents, pregnant and breastfeeding women, older Australians, Aboriginal and Torres Strait Islander peoples and culturally and linguistically diverse groups. Supporting educational resources for consumers and health professionals include the Australian Guide to Healthy Eating for the general Australian population and the new Aboriginal and Torres Strait Islander Guide to Healthy Eating. These resources provide visual advice on the proportion of the diet that should come from each of the five food groups each day.
In December 2014, the Australian Government launched the Health Star Rating system, which is a front-of-pack labelling system designed to help all grocery buyers make more nutritional choices when purchasing packaged foods. The system has been promoted through social marketing campaigns in December 2014, July–September 2015 and April–June 2016. All phases of the campaigns have incorporated specific media that targets Indigenous communities.
The Medical Outreach Indigenous Chronic Disease Programme (MOICDP) provides funding to support a wide range of health services that focus on the prevention, detection and management of chronic disease for Aboriginal and Torres Strait Islander people. MOICDP services include those provided by medical specialists, general practice, Aboriginal Health Workers, allied health workers and other health professionals. Access to nutrition and dietetic services in rural and remote areas are supported under the MOICDP.
In 2014, the Australian Government launched the Healthy Bodies Need Healthy Drinks resource package. This suite of culturally appropriate promotional materials encourages school-aged children, their families and communities to choose water instead of high-sugar drinks in an effort to prevent obesity, chronic disease and dental caries.
The Implementation Plan for the National Aboriginal and Torres Strait Islander Health Plan 2013–2023 recognises the importance of addressing the social and cultural determinants of health that contribute to poor dietary choices and poorer health outcomes, through coordinated whole-of-government action.
A range of state and territory initiatives are in place to address dietary behaviours. One example is the Move Well Eat Well which operates in primary schools and early childhood settings in Tasmania. This programme aims to improve the policies and practices in these settings to support nutrition and physical activity.
A description of policies and strategies relating to this measure are included in the Policies and Strategies section.