2.10 Community safety
Page content
Why is it important?
Experiencing threats of violence, being in an environment where personal safety is at risk, or in a social setting where violence is common, has negative health effects. The level of violence experienced by Indigenous Australians is also experienced in the context of colonisation, discrimination and subsequent markers of disadvantage such as low income, unemployment, lack of access to traditional lands and substance use (Day et al, 2013). Safe communities are places in which people are more likely to experience empowerment, security, pride, wellbeing and resilience (see measure 1.13).
Homicide and violence contributed 1.8% of the total burden of disease and injury for Indigenous Australians (AIHW, 2016f). A separate study on intimate partner violence found that it was responsible for 6.4% of the burden of disease and injury for Indigenous females, having its impact through anxiety, depression and suicide as well as homicide and violence (Ayre et al, 2016). Domestic/family violence is a major reason for seeking assistance from homelessness services (see measure 2.01) and also impacts child protection issues (see measure 2.12).
Findings
Based on the 2014–15 Social Survey, 22% of Indigenous Australians aged 15 years and over reported they were a victim of physical or threatened violence in the last 12 months, 2.8 times the rate for non-Indigenous Australians (8%). Actual physical violence was experienced by 13% of Indigenous Australians. Of these people, 71% reported that alcohol or other substances had contributed to the most recent violent incident they had experienced. Alcohol or other substances were more likely to have contributed in remote areas (77%) than non-remote areas (69%).
There has been no significant change between 2002 (24%) and 2014–15 (22%) for Indigenous Australians aged 15 years and over. Rates were similar for Indigenous females (22%) and males (23%). However, Indigenous females were more likely than males to report that they knew the offender of the most recent physical violence (96% compared with 83%). For Indigenous females who knew the offender, 39% were subject to violence by a current or previous partner and 48% by a friend or family member. Indigenous females were less likely to feel safe walking alone in their local area after dark (51% compared with 83% of Indigenous males) and were less likely to feel safe at home alone after dark (79% compared with 95% of males).
Indigenous Australians who were unemployed were more likely to report being a victim of physical or threatened violence than those who were employed (30% compared with 19% respectively). Those who had experienced being without a permanent place to live were twice as likely to report being a victim (31%) compared with those who had not (16%); and those living in a household in the lowest income quintile (26%) were more likely to report being a victim compared with those in the highest two quintiles (19%).
In 2014–15, there were similar rates across remoteness areas for self-reported experience of physical or threatened violence in the last 12 months; however hospitalisation rates show a different pattern. Data from 2013–14 to 2014–15 shows Indigenous hospitalisation rates for assault were highest in remote and very remote areas (22 and 21 per 1,000 respectively) compared with inner regional areas (3 per 1,000) and major cities (4 per 1,000). In non-remote areas, hospitalisation rates for assault were lower for Indigenous females than males but were higher in remote areas (26 per 1,000 and 18 per 1,000 respectively) and very remote areas (25 per 1,000 for females and 17 per 1,000 for males). The non-Indigenous female rate was lower than non-Indigenous males in all remoteness areas.
After adjusting for differences in the age structure of the two populations, Indigenous Australians were hospitalised for assault at 14 times the rate of non-Indigenous Australians. Indigenous females were 30 times as likely to have been hospitalised for assault as non-Indigenous females, and Indigenous males were 9 times as likely as non-Indigenous males. The Indigenous female rate was 53 times the non-Indigenous female rate in remote areas and 38 times in very remote areas. In the NT, rates for Indigenous females were 62 times the rates for non-Indigenous females. In 2014–15, Indigenous female family violence related hospitalisation rates were 32 times the rate for non-Indigenous females and the rate for Indigenous males was 23 times the rate for non-Indigenous males (SCRGSP, 2016b).
There has been no significant change in the rate of Indigenous hospitalisations due to assault between 2004–05 and 2014–15 in NSW, Vic, Qld, WA, SA and the NT combined. Rates of hospitalisation for assault were highest for Indigenous Australians aged 25–44 years. The most common injuries requiring hospitalisation were open wounds (29%) and fractures (28%). Home was the most common place of occurrence of the assault for Indigenous females (63%), particularly in non-remote areas (73%). For Indigenous males, common places were home (43%), street/highway (17%) or trade/service area (17%).
The 2014–15 Social Survey included questions on neighbourhood/community problems. Indigenous Australians living in remote areas were more likely to report problems involving youth (51%) than those living in non-remote areas (26%); alcohol (65% and 31% respectively); family violence (48% and 19% respectively); and assault (46% and 14% respectively).
As at 30 June 2016, the majority (63%) of Indigenous prisoners had been incarcerated due to violence related offences and offences that cause harm (see measure 2.11). In 2014–15, 48% of Indigenous males aged 15 years and over reported that they had been charged by the police in their lifetime, and 20% had been arrested by the police in the last 5 years. In 2014–15, 58% of Indigenous Australians aged 15 years and over reported they trusted the police from their local area and 46% trusted police from outside their local area, lower than the levels of trust in other sectors such as 81% of people trusting their doctor.
In 2015 (NSW, SA and the NT combined), police recorded 12,398 cases of assault where the victim was Indigenous. Indigenous females were more likely to be victims of assault than Indigenous men. Among non-Indigenous Australians, men were more likely to be victims of assault than women. For Indigenous females, partners were the most common offenders ranging from 38% of assaults in NSW to 57% in the NT. The Indigenous victimisation rate for assault was higher than non-Indigenous in all three jurisdictions, particularly for Indigenous women in the NT (11 times non-Indigenous women) and SA (9 times).
In 2011–15 there were 200 Indigenous deaths due to homicide. The mortality rate for homicide for Indigenous Australians was around 7 times the rate for non-Indigenous Australians. The Indigenous homicide mortality rate was highest among those aged 25–34 years, 10 times the non-Indigenous rate for this age group.
Between 1989–90 and 2013–14, 16% of all homicide victims were Indigenous. This is high given Indigenous Australians represent 3% of the Australian population. The majority (68%) of homicides, where both the victim and offender were Indigenous, were domestic homicides (partners or other family members). The equivalent was 44% for non-Indigenous Australians. Alcohol was involved for 68% of Indigenous victims and 70% of Indigenous offenders, much higher than for non-Indigenous victims (27%) and offenders (31%). Indigenous homicides increased by remoteness (from 76 in major cities to 509 in remote areas), while the number of homicides among non-Indigenous Australians decreased with remoteness.
Figures
Figure 2.10-1
Age-standardised hospitalisation rates for assault, by Indigenous status and remoteness, July 2013 to June 2015

Source: AIHW analysis of AIHW National Hospital Morbidity database
Figure 2.10-2
Deaths from assault (homicide) by Indigenous status and age, NSW, Qld, WA, SA and the NT, 2011–15
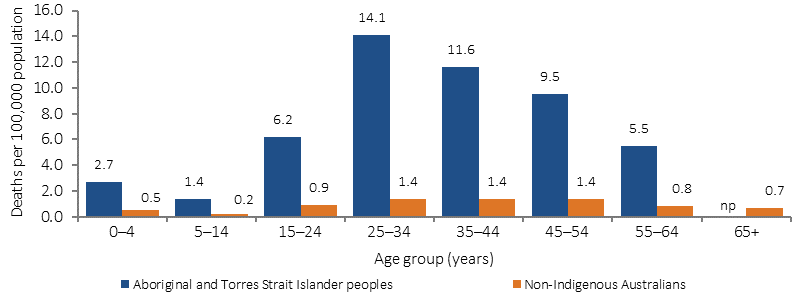
Source: ABS and AIHW analysis of National Mortality Database
Table 2.10-1
Experiences of violence, proportion of Indigenous Australians aged 15 years and over, by sex and remoteness, 2014–15
| Whether experienced physical or threatened violence in last 12 months | Males | Females | Non-remote | Remote | Australia |
|---|---|---|---|---|---|
| Percent | |||||
| Experienced physical or threatened violence | 23 | 22 | 22 | 23 | 22 |
| Experienced physical violence | 13 | 14 | 13 | 15 | 13 |
| Experienced physical violence more than once | 7 | 9 | 8 | 9 | 8 |
| Experienced threatened physical violence | 17 | 15 | 16 | 16 | 16 |
| Did not experience physical or threatened violence | 77 | 78 | 78 | 77 | 78 |
Source: ABS analysis of 2014–15 NATSISS
Figure 2.10-3
Male victims of assault, relationship to offender, by Indigenous status, NSW, SA & NT, 2015
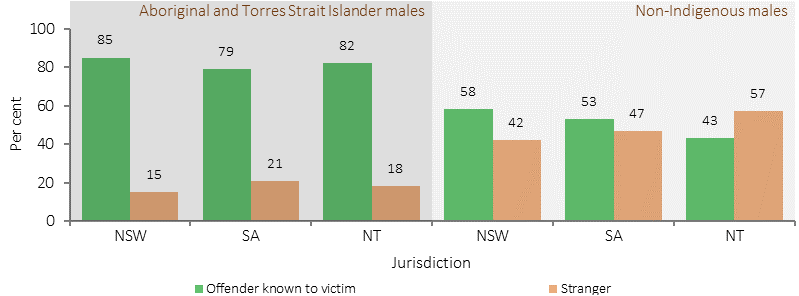
Source: ABS Recorded Crime —Victims, 2015 (ABS, 2016)
Figure 2.10-4
Female victims of assault, relationship to offender, by Indigenous status, NSW, SA & NT, 2015
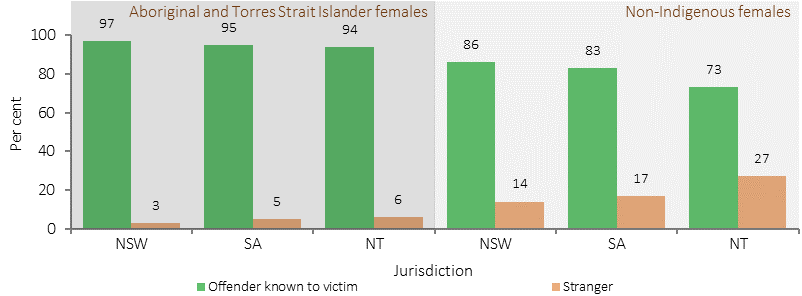
Source: ABS Recorded Crime —Victims, 2015 (ABS, 2016)
Implications
Having safe communities to live in is critical to closing the gap in Indigenous disadvantage. All Australian governments have endorsed the National Plan to Reduce Violence Against Women and their Children 2010–2022 (the National Plan), which includes a specific focus on domestic and family and sexual violence against Aboriginal and Torres Strait Islander women and their children through Outcome 3: Indigenous Communities Are Strengthened. The safety of Aboriginal and Torres Strait Islander women and children is a national priority area in the Third Action Plan of the National Plan. This plan will build upon the work of the previous two Action Plans focusing on improving services for victims of domestic and family violence, supporting community-driven initiatives to reduce or prevent violence and building capacity within the sector, including through workforce development.
The Australian Government’s Indigenous Advancement Strategy’s Safety and Wellbeing Programme seeks to enhance Indigenous community safety and wellbeing by funding activities on five key outcome areas: crime prevention, diversion and rehabilitation; violence reduction and victim support; reduced substance misuse and harm; improved individual and community health, wellbeing and resilience; and safe and functional communities.