3.15 Access to prescription medicines
Page content
Why is it important?
Essential medicines save lives and improve health when they are available, affordable, quality-assured and properly used (WHO, 2004). Affordable access to medicines is important for many acute and chronic illnesses. For chronic illnesses such as diabetes, hypertension, heart disease and renal failure, multiple medications may be required for many years to avoid complications (WHO, 2004). It is important to ensure that Aboriginal and Torres Strait Islander peoples, who experience high rates of acute and chronic illnesses, are able to access appropriate prescription medications when they are required. In Australia, the main mechanism for ensuring reliable, timely and affordable access to a wide range of prescription medications is the Australian Government’s Pharmaceutical Benefits Scheme (PBS). In 2014–15, the PBS subsidised the cost of 211.4 million prescriptions, at a cost of approximately $9.07 billion.
Findings
In 2013–14, total expenditure on pharmaceuticals per Aboriginal and Torres Strait Islander person was around two-thirds of the amount spent per non-Indigenous person ($579 compared with $857). In 2013–14, average expenditure per person for mainstream PBS benefits was $112 for Indigenous Australians and $338 for non-Indigenous Australians (in constant prices based on 2014-15 dollars). In 2011–12, average PBS expenditure per person for Indigenous Australians was estimated to be 23% of the amount spent for non-Indigenous Australians. In 2013–14 this was 33%. This suggests that the gap in spending between Indigenous and non-Indigenous Australians is closing. Note that changes over time may partly be explained by methodological changes and increases in Indigenous identification.
In 2013–14, mainstream arrangements accounted for 65% of benefits paid for Aboriginal and Torres Strait Islander peoples. The remainder were Section 100 and other special supply PBS drugs. The gaps between expenditures for Aboriginal and Torres Strait Islander peoples and non-Indigenous Australians were greatest in non-remote areas. In 2013-14, benefit-paid pharmaceutical expenditures for Aboriginal and Torres Strait Islander peoples were $131 per person in major cities, $137 for inner and outer regional areas and $305 for remote and very remote areas.
In 2014, the number of full-time equivalent pharmacists per 100,000 population declined with remoteness, from 84 per 100,000 in major cities to 51 per 100,000 in remote areas (AIHW, 2016c).
Results from a recent study show a reduction in hospitalisations for chronic conditions in areas with higher uptake of the PBS Co-Payment incentive (Trivedi et al, 2016). A multi-system coordinated approach through the including clinical care programmes is necessary for improving access to health care and reducing chronic disease (Bailie, J et al, 2015; Reed, 2017).
Figures
Figure 3.15-1
Pharmaceutical expenditure per person, 2013–14
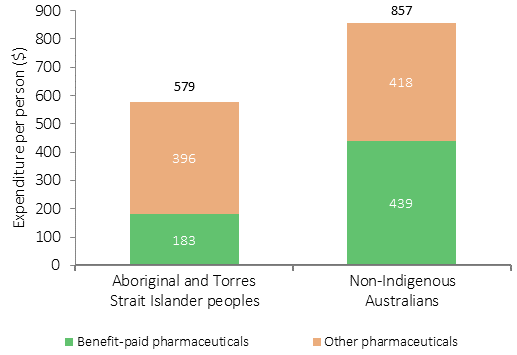
Source: AIHW health expenditure database (unpublished data)
Figure 3.15-2
Average health expenditure per person by the Australian Government on mainstream Pharmaceutical Benefits Scheme benefits, constant prices, by Indigenous status, 2011–12 to 2014–15
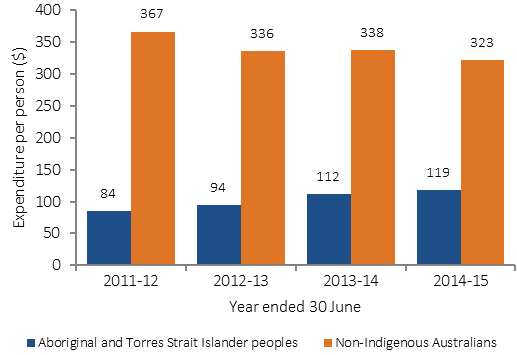
Source: AIHW health expenditure database (unpublished data)
Figure 3.15-3
Average health expenditure per person by the Australian Government on the Pharmaceutical Benefits Scheme,
by Indigenous status, 2013–14

Source: AIHW health expenditure database (unpublished data)
Implications
There is a large gap between PBS pharmaceutical expenditures for Aboriginal and Torres Strait Islander peoples and non-Indigenous Australians, although this gap appears to have reduced between 2011–12 and 2014–15. Estimation of this gap is complicated by the absence of high-quality data sources on Indigenous pharmaceutical usage and expenditures.
Access needs to be addressed at multiple levels. Prescription medicines are prescribed by primary care and specialist practitioners, and barriers to accessing these services in the first place may result in under use of medications. In 2012–13, 14% of Indigenous Australians reported that they needed to see a doctor but did not in the previous 12 months (see measure 3.14). Once a prescription has been issued, access to pharmacies may be limited, particularly in rural and remote areas. Financial barriers, particularly for people on low incomes, can be important, despite safety net schemes. It is estimated that in 2012–13, 34% of Indigenous Australians who did not fill a prescription gave cost as a reason. Ongoing compliance is important for all patients with chronic illnesses.
The following range of programmes and special arrangements allow intervention at multiple levels to improve access to PBS pharmaceuticals for Aboriginal and Torres Strait Islander peoples in both remote and non-remote areas.
Special supply arrangements administered under Section 100 of the National Health Act 1953 allow for PBS medicines to be provided to remote area Aboriginal and Torres Strait Islander primary health care services. The PBS medicines are dispensed to patients of the health care service by a suitably qualified and approved health professional, without the need for a prescription and at no cost. In 2015–16, $57.32 million was allocated towards Section 100 arrangements. This programme has played an important role in addressing medicines access problems in remote areas.
The PBS Co-payment Measure was introduced under the former Indigenous Chronic Disease Package on 1 July 2010 and continues to help address the financial barriers Aboriginal and Torres Strait Islander people may face in accessing PBS medicines in non-remote locations. These arrangements provide assistance with the cost of PBS medicines for eligible Aboriginal and Torres Strait Islander people living with, or at risk of, chronic disease. The identification of Indigenous clients is an important step in reaching the target population. The measure has been very successful to date, providing co-payment subsidies for a total of 407,861 eligible patients between 1 July 2010 and 30 June 2016, against an initial estimate of 76,000 patients, and subsidising 17.9 million PBS prescriptions.
Medicines are listed on the PBS on recommendation of the Pharmaceutical Benefits Advisory Committee (PBAC). The PBS listing process is based on evidence. Under the National Health Act 1953, the PBAC must consider each PBS listing application having regard to the clinical effectiveness and cost effectiveness of the medicine for the intended medical use. Availability of PBS medicines is for all Australians but can vary, where some medicines can be restricted access.
Under the relevant regulations, cost recovery fees for applications to the PBAC may be waived when the application is in respect of medicines for Aboriginal and Torres Strait Islander peoples.
Under the 6th Community Pharmacy Agreement funding is provided to assist pharmacies operating in rural and remote areas through the Rural Pharmacy Maintenance Allowance. Programmes specific to Indigenous health have also been funded including the Quality Use of Medicines Maximised for Aboriginal and Torres Strait Islander People program. The primary aim of this programme is to improve medication compliance and quality use of medicines and consequently the health outcomes of Aboriginal and Torres Strait Islander people that attend participating Aboriginal Community Controlled Health Organisations in rural and urban areas of Australia.
The Pharmaceutical Society of Australia’s Guide to providing pharmacy services to Aboriginal and Torres Strait Islander people (PSA, 2014) was released in 2014 to assist pharmacists and pharmacy staff to be responsive to health beliefs, practices, culture and linguistic needs of Aboriginal and Torres Strait Islander people, families and communities. The guide encourages increased engagement with Indigenous health services and key Indigenous organisations and includes an overview of Aboriginal and Torres Strait Islander specific medicine programmes and a resource list from which pharmacists can gather more in-depth information.
It is important to develop a better understanding of how the various barriers impact on Indigenous Australians to better target strategies. As data improve, better analysis of gaps in the PBS arrangements will be possible to inform programmes and policies.